In September, we talked about my high school English teacher, Janie.* She had developed lymphedema due to her cancer but also had other contributing factors to her lymphedema development. Let’s continue with additional contributing factors to her lymphedema development. We’ll also see how she managed her swelling over the years. Read Part 1 here.
Diuretic Use
Lasix was prescribed as a treatment for Janie’s leg swelling most likely in 1982. Lasix is a diuretic used to get rid of excess fluid. Diuretics are a contraindication for the treatment of lymphedema when that is the sole condition being treated. 3 The reason is while diuretics do help get rid of excess fluid by increasing urine output, they cause hemoconcentration (an increase in the concentration of what’s in blood other than fluid – like the protein mentioned previously). The lymphatic system transports several items from the tissue. One of those items happens to be protein.
Protein attracts water. If the lymphatic vessels of an extremity are damaged and proteins are accumulating in the tissue, what happens? Fluid begins to accumulate (swelling). The definition of lymphedema is an accumulation of protein-rich fluid caused by a structurally impaired lymphatic system. As protein, fluid & other matter that the lymphatic system normally transports remain in the tissue, inflammation develops. This leads scarring or fibrosis (hardening) as the body remodels the tissue. This process causes the tissue to become firmer over time & creates more congestion.
Cancer return

In 1984, Janie admitted to the hospital with shortness of breath & chest pain.
She was found to have a pleural effusion (a buildup of fluid between the lung(s) & the outer lining), atelectasis (partial lung collapse), pericardial effusion (fluid around heart), enlarged chest lymph nodes and a mass in her chest. As a result of the fluid around her heart, she developed pericardial tamponade (a condition which prevents the heart from fully refilling). Blood pressure can drastically drop & cause death. She had an emergency procedure in which the surgeon cut into her chest between the ribs to access the heart. Once there, a cut was made into the lining of the heart to drain the excess fluid. A biopsy of the mass was done & chest tubes were inserted to allow draining after surgery. The biopsy revealed lymphoblastic lymphoma. Six months of chemo, radiation to her head & several spinal chemo injections later, Janie recovered & remained in cancer remission for several years.
Lymphedema
Non-pitting, chronic lymphatic obstruction
Medical records (below) describe the swelling in her left ankle as not being painful. Other than the early stage of congestion, lymphedema is generally not painful. (An exception may be when there is edema & lymphedema.) The spongy pitting becomes firmer over time until an indentation can no longer be made, & eventually, swelling no longer reduces with elevation. In 1987, a doctor’s letter describes Janie’s lymphedema as non-pitting, extending from the groin to the foot, lymphatic-obstruction, and not reversible. She is prescribed a pump.
Intermittent Pneumatic Pump
Dennis (Janie’s husband) described this pump as one that encompassed her leg only (no trunk component) & started pumping from the foot & continued up the leg. This is a typical sequential that can be helpful for venous insufficiency, but it isn’t the right pump for lymphedema. In fact, it can worsen lymphedema instead of improve it.4 Here’s why:
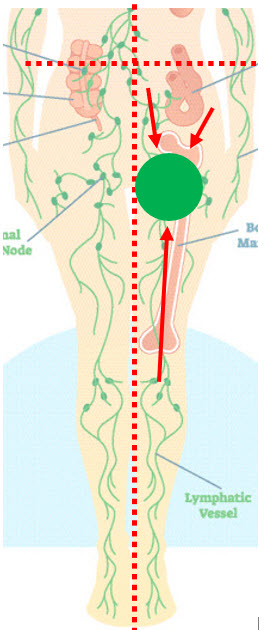
In cases of lymphedema, a quadrant of the trunk is usually involved in addition to the swollen extremity.
Both the quadrant & extremity drain to the same lymph node region. In Janie’s case, her left leg & left lower quadrant of her trunk would have been involved. These areas drain to the same area (the left inguinal lymph nodes). If a pump leg sleeve stops near the thigh, fluid is just pushed the drainage region that is already impaired. Janie’s pump was prescribed in the 1980s, but lymphedema patients today are often prescribed a similar pump.
While the pump may decongest the leg temporarily, it ends up pushing fluid (& shifting pressure) to the already congested area of trunk quadrant & inguinal lymph nodes. In cases of leg lymphedema, fluid may even be shifted into the genitals. If it backs up into the trunk quadrants, a fibrosclerotic wall develops. Foldi’s Textbook of Lymphology outlines additional concerns: worsening lymphedema, removing more water than protein & increased pulmonary blood capillary pressure.5
Recommended pumps will have an abdominal trunk component & initiate a proximal massage before pumping. Ideally, these pumps will decongest the trunk, upper thigh, lower, thigh, knee, upper lower leg & lower leg (in that order) before beginning to push fluid from the foot up. This “sort of” mimics the manual lymph drainage sequence & decongests the area before pushing fluid into it from the swollen leg.
Compression Garment
In 1997, a physician wrote a letter that summarized Janie’s status. They noted that she wore TED hose & used ACE bandages. If she really was using ACE bandaging, she would see some improvement but not as good as she would with traditional multi-layer, short-stretch lymphedema compression. ACE wraps are long-stretch bandages which have more elasticity & give under resistance. They don’t provide the working pressure short-stretch bandages do to remove fluid from the tissue as a person uses their muscles. Some patients also do not tolerate long-stretch as well.

The compression hose she used per this note were TED hose.
TED hose are anti-embolism hose often used in hospitals after surgery. They have 15-20 mmHg which isn’t typically enough compression for cases of leg lymphedema. Generally, if there is no arterial blood flow impairment or other concerns, compression of 30-40+ mmHg are used on a leg to overcome pressure in the tissue caused by gravity. I know Janie never obtained a custom, flat-knit hose when I was in school (the recommended garment). She used a circular-knit hose which looks similar to a pantyhose & don’t provide the same benefits that custom, flat-knit hose do.
Lymphedema Treatment
Janie did attend a lymphedema clinic in St. Louis in the late 1990s / early 2000s (which was an hour & a half away from her home – the nearest one). Lymphedema treatment includes a massage called manual lymph drainage (MLD), multi-layer short-stretch bandages, exercise & skin care. Records reveal insurance began paying for MLD in the late 90s. I’m hopeful she may have eventually gotten better care for her lymphedema.
Breast cancer, traffic, blood clot & pelvic cancer
In 1997, she noticed a small nodule in her right breast, but doctors were not concerned. They wanted to monitor it. However, between June of 1999 & July 2000, she was diagnosed with ductal carcinoma in situ (breast cancer). She had a lumpectomy & was prescribed Tamoxifen which appeared to resolve her breast cancer. In 2002, she was stuck in traffic for three hours & began having leg pain. She went to the emergency room & was found to have a DVT (blood clot) in her left leg with significant increased swelling.
She was evaluated by Mayo Clinic for her lymphedema soon after. The doctor stopped lymphedema massage (due to the DVT) but had her continue compression on her leg. According to notes, she never used night compression as a part of her maintenance routine. (Day & separate night compression should be a part of lymphedema maintenance. Without night compression, the leg often refills.)
In 2003, Janie was diagnosed with pelvic cancer. In 2004, she decided to retire a year early & spend time with her family & enjoy traveling (to Ireland, Turkey, the Pacific Northwest…). She saw her son get married, & she met her first grandbaby – no doubt two of the biggest joys of her life. In 2006, the pelvic mass was described as encompassing her common iliac blood vessels & ureter. She received radiation to her pelvis with some improvement (including some leg swelling improvement likely due to tumor shrinkage). In 2009, Janie lost her battle with cancer.
Continued to live a full life
From the beginning of her first cancer diagnosis, Janie kept excellent records allowing me to follow her journey through cancer, treatment, recurrence & complications. Even though she didn’t dwell on her problems, her notes gave me insight into what she was might have been thinking at times as she oriented to the medical terms with self-education. Titles of some of her printouts included:
- side effects of chemo: hair loss, low WBC count, neuropathy, joint pain, muscle pain, cardiac effects, local irritation, low RBC count, stomach upset, diarrhea
- information about metastatic cancer
I can only imagine the self-consciousness a person experiences losing their hair let alone the fear that can come from a diagnosis of cancer. No doubt she struggled with the diagnoses she faced. She had several setbacks besides those already mentioned. Over the years she also experienced chronic anemia; short-term facial swelling; acute Bell’s Palsy; enlarged spleen; mild, chronic left hip pain from bursitis (& likely from the weight of her swollen leg); a blocked ureter (impeding urine flow from one kidney to the bladder); a failed ureter stent placement; urinary tract infection(s); shingles & a severe pelvic infection which became septic — & that isn’t all. I had no idea what she went through. She dealt with these challenges with strength & dignity. Never once do I recall her complaining. Dennis said she wasn’t one to focus on herself or her problems. Instead, she chose to face the obstacle, seek resolution or management, do what was best for her family & focus on living.
This series is dedicated to “Janie” & all those who are managing lymphedema caused by cancer.
~Janie~
(11/01/50 – 3/12/09)
I’ll be featuring my interview with Dennis in the coming YouTube channel. Stay up-to-date on development by joining the conversation.
References
1 Bankov K, Döring C, Ustaszewski A, Giefing M, Herling M, Cencioni C, Spallotta F, Gaetano C, Küppers R, Hansmann ML, Hartmann S. Fibroblasts in Nodular Sclerosing Classical Hodgkin Lymphoma Are Defined by a Specific Phenotype and Protect Tumor Cells from Brentuximab-Vedotin Induced Injury. Cancers (Basel). 2019 Oct 30;11(11):1687. doi: 10.3390/cancers11111687. PMID: 31671543; PMCID: PMC6896072. Available from: https://pubmed.ncbi.nlm.nih.gov/31671543/.
2 Kamal MM, Khude SR, Yadav SB, Raut WK, Pangarkar MA. Syncytial variant of nodular sclerosing Hodgkin’s disease: A diagnostic pitfall in fine-needle aspiration cytology. J Cytol. 2014;31(2):91-92. doi:10.4103/0970-9371.138674. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4159904/.
3 Foldi, M, Foldi, E. (2006). Foldi’s Textbook of Lymphology (2nd ed.), p. 282-283, 446. Germany: Urban and Fisher.
4 Foldi, M, Foldi, E. (2006). Foldi’s Textbook of Lymphology (2nd ed.), p. 282. Germany: Urban and Fisher.
5 Aldrich MB, Gross D, Morrow JR, Fife CE, Rasmussen JC. Effect of pneumatic compression therapy on lymph movement in lymphedema-affected extremities, as assessed by near-infrared fluorescence lymphatic imaging. J Innov Opt Health Sci. 2017;10(2):1650049. doi:10.1142/S1793545816500498

Ask A Therapist