We’re continuing a patient story from last month. (Click here for part 1)
The patient we’ve been following received a daytime CCL 2 sleeve & glove (she also wanted to try a gauntlet). She also received her CCL 1 sleeve & glove which she wanted to try for night use (instead of the recommended protocol of bandaging or a foam sleeve).
What Happened?
Five weeks after getting her daytime sleeve/glove, she had issues with finger swelling & arm refilling. She wasn’t resting well at night either. She stopped using the CCL 1 garment & used the same CCL 2 sleeve at night. When she returned to see me, she seemed angry (with me) for her outcome. When there’s a deviation from the protocol, the outcome will be affected.
I noted the likelihood of using a CCL 2 daytime sleeve/glove at night, especially when sleeping with elbow bent, as contributing to her forearm swelling & worsening fibrosis. While resuming bandaging was the best idea, she was adamant she wasn’t going to do that again. I said the next best option would be to get a nighttime foam sleeve. It should help reduce the forearm fibrosis which would help reduce the swelling. She agreed.
(collaboration with a local garment rep on best night garment in this case)
Intervention
This patient chose to continue wearing her daytime CCL 2 sleeve/glove (23-32 mmHg) before being fit for the night garment. (She hadn’t been re-reduced with bandaging.) That meant, the nighttime garment would likely be bigger than it should be. The fitter tried to compensate for this by decreasing the circumferences. (I had the manufacturer’s local rep do the fitting.)
Outcome
It took several weeks for the nighttime garment to arrive. The patient continued wearing the CCL 2 sleeve & glove during this time. (She did come in for bandaging one session prior to the arrival of the night garment.) The night garment was a little short & a little big, but the patient agreed to try it at night. After a few nights, she felt she was doing well & seeing progress.

(photo sent by pt after removing the night garment in the morning; she had worn it several nights)
When she returned to see me, she was happy with her status. Because the night sleeve wasn’t quite as long as it could have been (or the patient hadn’t been able to keep it up near the shoulder because it was a too large around the upper arm), there was some refilling around the shoulder. But her other numbers were improved as her fibrosis softened with the chipped foam sleeve.
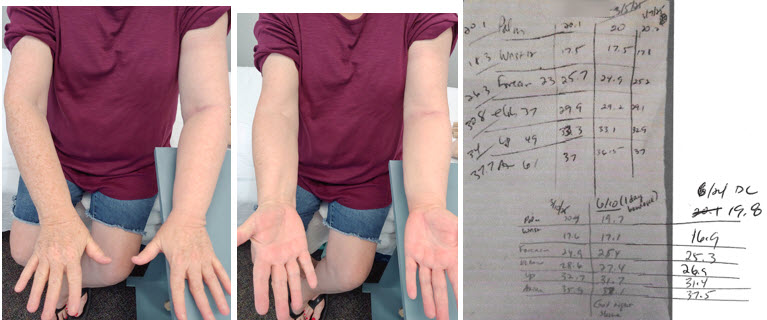
(final visit after wearing night foam sleeve: volume 26.3 cm)
Can You Cheat the System?
Short answer: No. The protocol for lymphedema treatment exists to maximize the best outcome by softening fibrosis & decongesting tissue. Once this process is complete, a patient is ready for their maintenance day & night garment fitting. They should remain bandaged until both garments are in place.
This patient’s course was prolonged & a bumpy ride to get to her conclusion. But in the end, she was happy with her status. That’s what matters most. Sometimes a patient’s goals aren’t solely to maximize reduction. Convenience or interference with daily routines may trump the “ideal outcome.” It’s important to ask a patient what their goal is & to monitor this goal during the course of therapy as it may change.