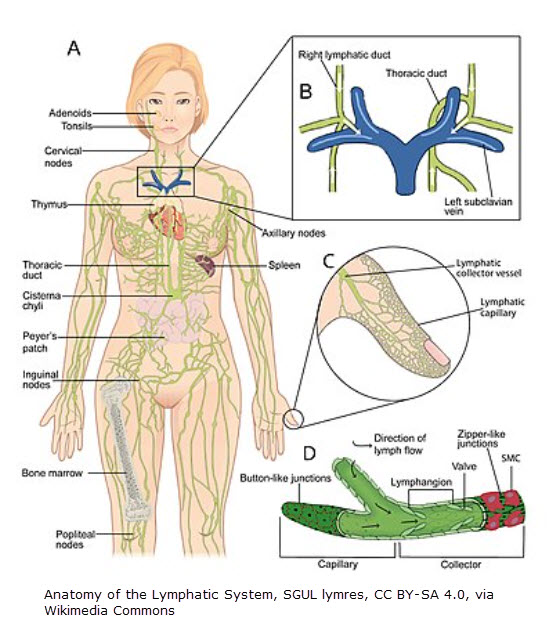
Researchers at Yale are studying the lymphatics discovered in the meningeal dura mater. Anne Eichmann, Professor of Medicine said, “Meningeal lymphatic vessels are potential targets to treat brain diseases.”1 This includes causes of intracranial hypertension like brain injury or stroke according to Foldi.2
Foldi had it going on
Years before Yale’s 2022 research, Foldi had written about this in the Foldi Textbook of Lymphology. In the chapter on lymphostatic diseases, Foldi notes lymphostatic failure can occur in the body’s organs – including the brain. Many people might consider this “lymphedema.” But lymphedema is referring to the lymphostatic condition that affects the skin & tissues. When it’s elsewhere in the body, it’s simply called “lymphostatic failure.” If it affects the nerves, it’s called, “lymphostatic neuropathy.” If it affects the brain, it’s called, “lymphostatic encephalopathy.” Etc. Foldi states, “Any organ requiring lymphatic drainage develops a lymphostatic disease under circumstances of low-output failure or combined [high & low output] failure.”2
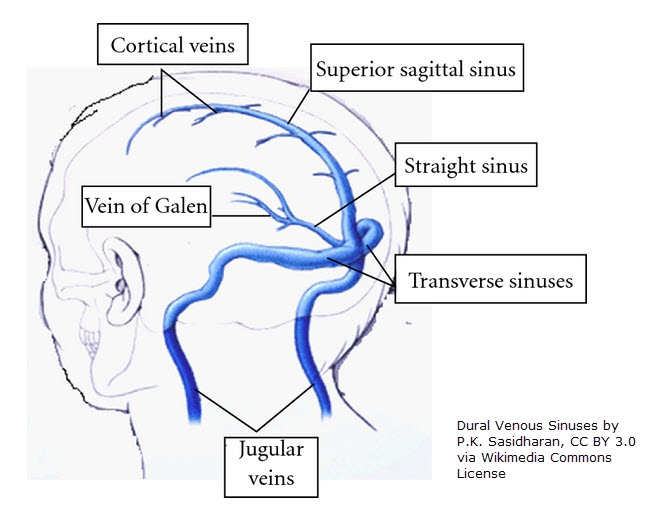
What can give rise to congestion surrounding nerves? Inflammation, as occurs in trigeminal neuralgia (cranial nerve V is affected) & Bell’s Palsy (the facial nerve, cranial nerve 7, is affected). Cranial nerve V runs through the dural venous sinus (the cavernous sinus). Cranial nerve 7 passes through the temporal bone. There’s a head & neck MLD sequence that can address this.
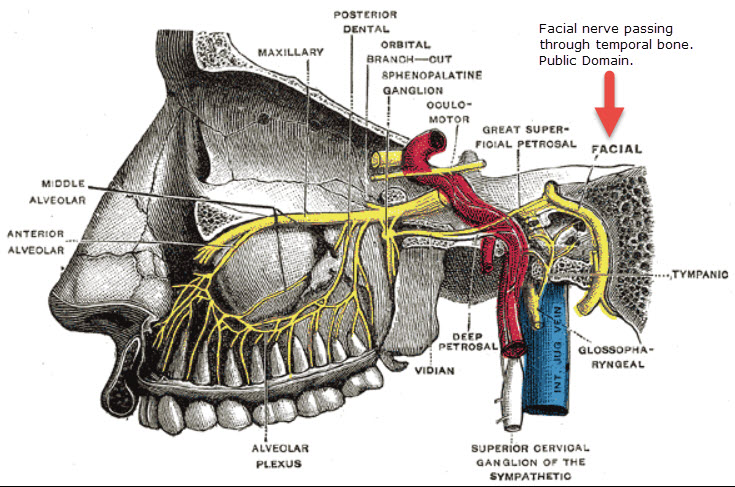
On the right is the facial nerve involved in Bells’ Palsy. The picture shows it passing through the temporal bone. The nerve can swell, causing it to be compressed. This leads to the symptoms people experience.
Why direction matters
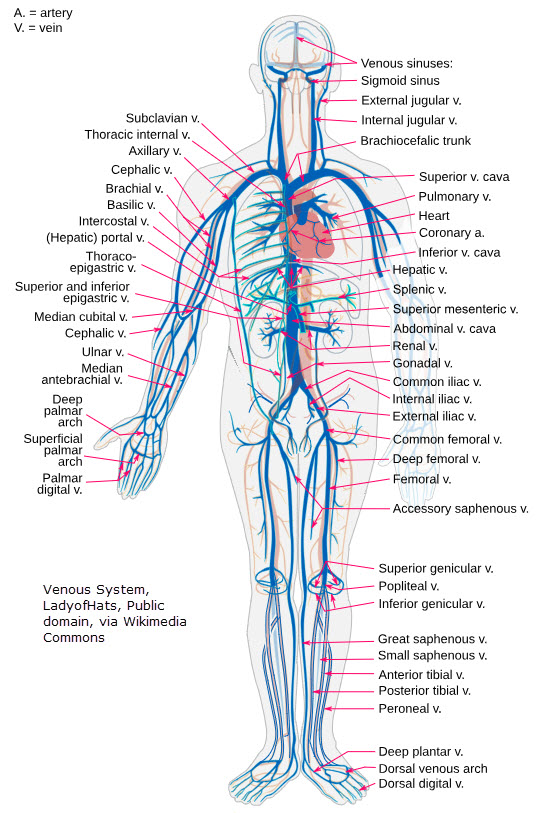
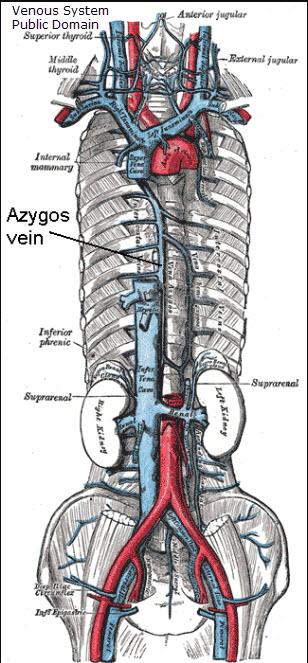
It’s important to be aware that dural venous sinuses don’t have valves or muscle like regular veins do. As a result, blood can flow backwards. In fact, most brain veins (except for the larger pial veins) don’t have valves or muscle.3 (Spinal veins are also valveless & muscleless.4)
The missing valves & muscle in these veins allows them to expand if intracranial pressure rises. But, as The Noted Anatomist states, “Veins that drain the eyes or nasal pages could flow backwards, back into the orbit or nasal area. This could transport infection into the brain.” That’s the downside. MLD may be able to help this backflow caused by congestion.
How MLD could help
Foldi notes that, “Immune deficiency develops in lymphedematous areas. This fact plays an important role in the pathophysiology of lymphostatic diseases.”5 In lymphedema, as inflammation continues, we see the changes characteristic of lymphedema tissue as the disease progresses (skin thickening, fat growth, scarring or fibrosis, skin papules & hyperkeratosis, etc.). Complete decongestive therapy (with MLD being one of the components of CDT) improves this condition by decongesting the tissue. It’s a proven fact that proper MLD speeds up lymphatic flow.6,7,8 Check out the below video of a person receiving leg MLD. It shows the movement of lymph fluid before & after MLD.
If MLD can increase lymph transport, it stands to reason that it could reduce swelling around nerves or congestion in the brain given what we’ve learned about anatomy. Foldi has already suggested that it does. Wolf Lüdemann (physician) treated patients with intracranial pressure due to brain injury using MLD. And the pressure reduced.9 (It’s important to note position can also play a role in intracranial pressure.)
Foldi highlighted patients with recurrent inflammatory nasal congestion & primary lymphedema (which caused dysplasia of the jaw & paranasal sinuses) who were treated with MLD. Their tonsils were often enlarged, leading to mouth-breathing. The kids often have trouble staying awake & concentrating in school. Colds were a common occurrence. MLD improved their symptoms.10
The start of modern MLD
It’s interesting to note that Dr. Emil Vodder (credited with being the founder of MLD) got his start in the south of France treating patients with colds, migraines & sinus problems.11
Conclusion
MLD has potential to help nerve inflammation & conditions causing intracranial pressure through head & neck MLD. In fact, “Földi’s concept of lymphostatic encephalopathy provides both a possible explanation of the wide spectrum of symptoms after these accidents [causing increased brain pressure] and a way to help heal the problems by using MLD.”12
References
1 https://medicine.yale.edu/news-article/the-brains-drainage-system-in-3-dimensions/
2 Földi, Michael; Földi, Ethel; Strößenreuther, Cornelia; Kubik, Stefan. Földi’s Textbook of Lymphology: for Physicians and Lymphedema Therapists (German Edition) (p. 515). Elsevier Health Sciences. Kindle Edition.
3 Hufnagle JJ, Tadi P. Neuroanatomy, Brain Veins. [Updated 2023 Jul 24]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-. (https://www.ncbi.nlm.nih.gov/books/NBK546605/#:~:text=Structurally%2C%20the%20veins%20of%20the,a%20circumferential%20smooth%20muscle%20layer)
4 (Green K, Reddy V, Hogg JP. Neuroanatomy, Spinal Cord Veins. [Updated 2023 Jul 24]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-. https://www.ncbi.nlm.nih.gov/books/NBK542182/)
5 Földi, Michael; Földi, Ethel; Strößenreuther, Cornelia; Kubik, Stefan. Földi’s Textbook of Lymphology: for Physicians and Lymphedema Therapists (German Edition) (pp. 515-516). Elsevier Health Sciences. Kindle Edition.
6 https://ltstherapy.com/blog/can-mld-slow-cognitive-decline-part-3/
7 Tan IC, Maus EA, Rasmussen JC, et al. Assessment of lymphatic contractile function after manual lymphatic drainage using near-infrared fluorescence imaging. Arch Phys Med Rehabil. 2011;92(5):756-764.e1. doi:10.1016/j.apmr.2010.12.027 (https://pmc.ncbi.nlm.nih.gov/articles/PMC3109491/)
8 https://www.movinglymph.com.au/post/update-on-icg
9 Földi, Michael; Földi, Ethel; Strößenreuther, Cornelia; Kubik, Stefan. Földi’s Textbook of Lymphology: for Physicians and Lymphedema Therapists (German Edition) (p. 716). Elsevier Health Sciences. Kindle Edition.
10 Földi, Michael; Földi, Ethel; Strößenreuther, Cornelia; Kubik, Stefan. Földi’s Textbook of Lymphology: for Physicians and Lymphedema Therapists (German Edition) (p. 712). Elsevier Health Sciences. Kindle Edition.
11 https://vodderschool.com/emil_vodder_life_work_article
12 (Földi, Michael; Földi, Ethel; Strößenreuther, Cornelia; Kubik, Stefan. Földi’s Textbook of Lymphology: for Physicians and Lymphedema Therapists (German Edition) (p. 1844). Elsevier Health Sciences. Kindle Edition.)