(Part 3)
In this final post on arm use after breast cancer, we’ll take a look at research-backed strengthening. But first, an announcement.
Announcement
The Lymphedema Treatment Act (LTA) passed Congress3 just before Christmas (passing the House of Representatives – Bill H.R. 3630 on 11/17/221 & Senate – Bill S.1315 on 12/23/222). This means compression garments will be covered by Medicare. Say thank you to your congressmen & women by sending an email here.
Research Says
According to research, how should you safely, progressively strengthen your arm to avoid causing or exacerbating lymphedema? (Disclaimer: This is my general conclusion of the articles I reviewed. Be sure to ask your certified lymphedema therapist what the best protocol is for your situation before engaging in any exercise. Proper form is important, and you should not experience pain with exercise. Stretching & strengthening should be done slowly and with control.)
Step One – Warm Up and Stretch
According to the Pal study,1 participants started with 10 minutes of cardiovascular warm-up followed by brief stretching of the muscles to be strengthened.
Step Two – Focus on the Core
Participants then did 5-15 minutes of core strengthening (spine stabilizing and abdominal exercises) to prevent injury during arm strengthening.
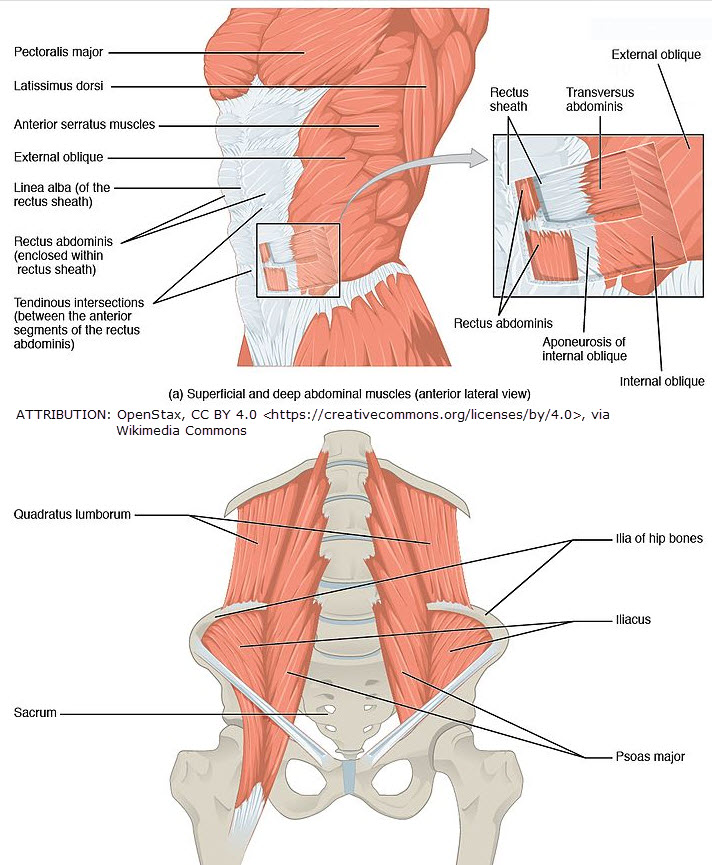
There are 29 pairs of muscles that make up the core.4 The study doesn’t specify which core muscles were targeted. But I anticipate these would include the glutes and paraspinal muscles,2 transverse abdominus, quadratus lumborum and obliques.
According to a Sports Medicine article,4 proper core strengthening might start with:
- Cat camel (or cat cow) stretch. This is a common Yoga stretch done in a quadruped position on the hands and knees.
- Abdominal bracing variations (it’s important to properly engage the abs through abdominal bracing exercises before advancing core exercise).
- Bird dog pose (alternating arm and leg lifts in quadruped) or planks to engage paraspinal muscles. Modified versions of side planks (such as standing side trunk flexion) might be added to engage quadratus lumborum and obliques before doing floor side planks. (For a more robust and difficult core-strengthening program, visit here.3 But know that many people will need to start with easier, modified versions.)
The number of repetitions will vary according to a person’s fitness and status. Anywhere from 5-10 reps of each is a good place to start and working up to 15 reps.
Step Three – Strengthening
Start with no weight or 1 lb. (You can also use a low-resistance Theraband.) If there are no changes in symptoms or lymphedema-onset by the next week, increase weight by 0.5 or 1 lb.

(Two 2 Kg. weights image licensed under Creative Commons Zero by Pixabay/Pexels)
The goal is to reach 3 sets per exercise* in the first 3-4 weeks. As a general rule, increase weight after 4 consecutive sessions lifting the same weight for 10, 10, and 12 reps for sets 1, 2, and 3, respectively.1
- Tips:
1. If there are changes in symptoms, the exercise thought to be causing the problem should be skipped or a lighter weight should be used until symptoms clear up.
2. If 2 sessions are missed, deconditioning may result. Resistance should be reduced and gradually increased as outlined above.
3. Monitor symptoms weekly for changes indicating decline (i.e. swelling, tightness, discomfort, etc.) and measure monthly1 (or more often if you want to be more vigilant).
*Exercises might include: Chest press, lat pull-down, bicep curl, triceps extension, lateral arm raise, wrist curl 5 among others.
Step Four – Repeat Step One with Cool Down Stretching (hold positions for 30 seconds)
References (blog)
1 Schmitz KH, Troxel AB, Cheville A, et al. Physical Activity and Lymphedema (the PAL trial): assessing the safety of progressive strength training in breast cancer survivors. Contemp Clin Trials. 2009;30(3):233-245. doi:10.1016/j.cct.2009.01.001
2 https://www.healthline.com/health/paraspinal-muscles#takeaway
3 https://www.mayoclinic.org/healthy-lifestyle/fitness/multimedia/core-strength/sls-20076575
4 https://journals.lww.com/acsm-csmr/Fulltext/2008/01000/Core_Stability_Exercise_Principles.14.aspx
5 Cormie P, Singh B, Hayes S, et al. Acute Inflammatory Response to Low-, Moderate-, and High-Load Resistance Exercise in Women With Breast Cancer-Related Lymphedema. Integr Cancer Ther. 2016;15(3):308-317. doi:10.1177/1534735415617283
References (Lymphedema Treatment Act)
1 https://www.congress.gov/bill/117th-congress/house-bill/3630
2 https://www.congress.gov/bill/117th-congress/senate-bill/1315/text
3 https://buddycarter.house.gov/news/documentsingle.aspx?DocumentID=10733


