Last month, we began a series on contraindications to MLD. This post will continue that topic, citing a few more contraindications.
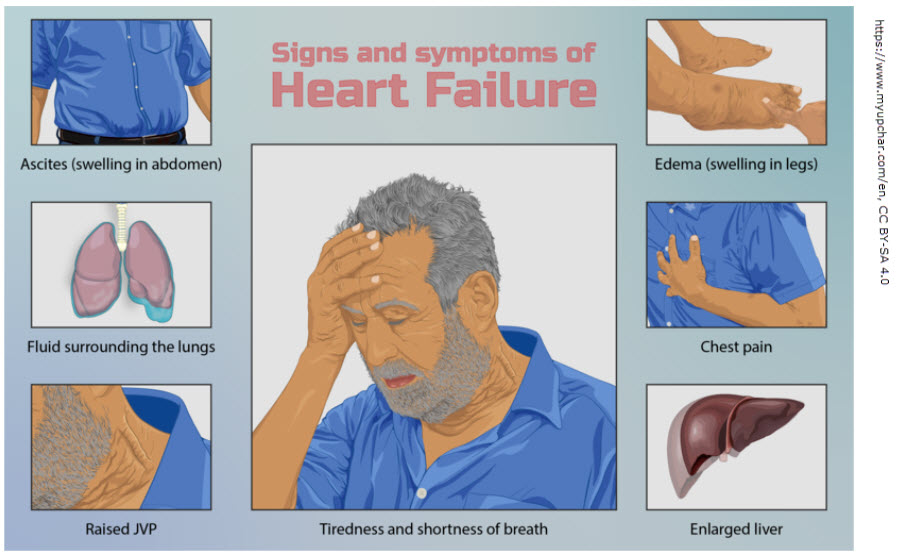
3. Heart Failure
Patients with heart failure are at risk for fluid overload, and MLD could further strain their cardiovascular system. The technique’s effects on fluid mobilization may overwhelm the heart’s ability to manage the increased fluid load. Foldi underscores the importance of careful evaluation of a patient’s cardiac function before initiating MLD, especially in those with advanced heart conditions. MLD is not appropriate if heart failure isn’t controlled. And it’s not appropriate if the sole reason for swelling is heart failure as that is a medical condition requiring medical intervention (not lymphedema). Patients with combined edema (from heart failure or other organ dysfunction) and lymphedema require extra caution.
4. Renal Insufficiency
Patients suffering from severe renal insufficiency or kidney failure may experience difficulties in fluid regulation. In such cases, MLD could cause fluid retention and exacerbate symptoms like edema or ascites (according to Ai). (My position is that MLD increases lymphatic flow & ultimately cardiovascular return & renal load. But MLD is primarily not done as it would be of no benefit because lymph vessels are already working at maximum capacity due to the dynamic nature of the edema.) Patients with impaired kidney function should be closely monitored, and MLD should be avoided or used with extreme caution in individuals with compromised renal status. Again, patients with combined edema (from renal disease or other organ dysfunction) and lymphedema require extra caution.
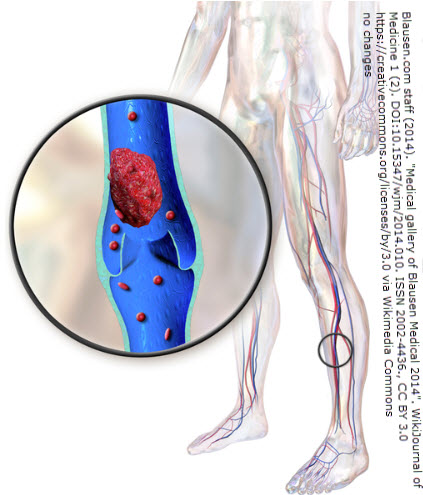
5. Thromboembolic Disorders
Deep vein thrombosis (DVT) or other thromboembolic disorders are a significant contraindication for MLD. Manual lymph drainage can increase blood and lymphatic flow, potentially dislodging clots and causing a pulmonary embolism (PE) or other complications. Foldi’s Textbook emphasizes the critical importance of excluding thrombosis prior to MLD treatment and recommends that patients with active DVT or a history of thromboembolic events within 6 months not undergo MLD (with some exception). DVTs in the acute phase are at risk of dislodging & creating a PE which can kill a person. In the subacute phase (which occurs over the next several weeks), there is typically pain, redness and swelling. The body begins to break down the clot in a process known as fibrinolysis, where enzymes dissolve fibrin and other clot components. As this process happens, part of the clot is reabsorbed, while the remaining structure becomes more organized and fibrous. In the chronic phase (month 3-6), the clot typically becomes firm and organized (restructured with scar tissue) and has little risk of dislodging by month 6.
The exception to waiting 6 months is if a person has a filter and/or receives anticoagulation medication. After stabilization with anticoagulant therapy, MLD may be safely resumed after a 2 to 4-week period (if the physician approves MLD).
Generated by Ai (with edits by author)
References
Foldi’s Textbook of Lymphology
*****For Medicare garment coverage updates, click here.*****