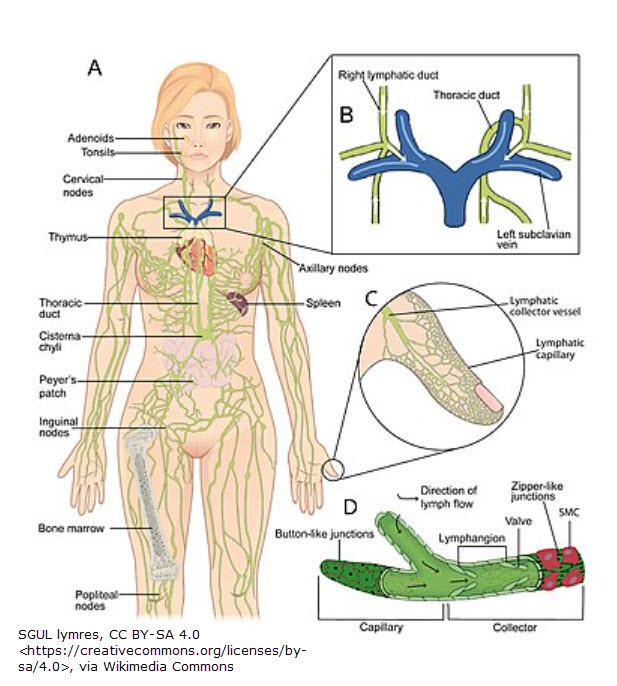
Even though the legislation was submitted over 10 years ago to government delegates, the Lymphedema Treatment Act is still not widely recognized by most people who have lymphedema. Yet passage of the bill (which was accomplished Dec. 23, 2022) is so important to lymphedema care. It will become effective Jan. 1, 2024. Why is it important to lymphedema?
Lymphedema Care
Lymphedema treatment has two phases. Phase I is decongestion. This is the therapy phase when CDT is administered. (CDT is complete decongestive therapy & involves manual lymph drainage, bandaging, skin care & exercise.) Once maximum reduction is attained in therapy, the next step is fitting with a compression garment (usually for day & night). This is a part of Phase II (the maintenance phase).
Maintenance Phase
Compression garments are mandatory for lymphedema maintenance. Without them, swelling will promptly recur, & the reduction obtained during therapy will be lost. There are a few different types of compression.
- Flat-knit (usually custom-made, but readymade is available) – daytime garment
- Circular-knit (usually readymade, but custom is available) – daytime
- Velcro (commonly used in wound care or as a night option) – day or night
- Foam sleeves (nighttime use) – night
(Note: Self-bandaging at night is the textbook recommendation for lymphedema maintenance.)
Recommended Compression
While circular-knit & Velcro can be used in some edema-related cases (such as venous edema) or combination edema-lymphedema cases (such as phlebolymphedema), the recommended compression for lymphedema is custom, flat-knit. One reason is the fact the many lymphedematous extremities don’t fit into the readymade dimensions. Another reason is the way flat-knit garments are made. While other garments provide compression, flat-knit provides the best containment. Flat-knit also aids in softening hardened, fibrotic tissue caused by lympedema. Finally, flat-knit is a thicker fabric less prone to bunching & causing pain in joints (such as ankles & behind knees).
Cost & Insurance
The downside to compression is cost. Compression should be replaced every 6 months (to a year) because it loses its effectiveness as fibers wear out.1 Many insurance carriers follow Medicare’s guidelines, & until 2024, Medicare won’t cover the cost of lymphedema compression. Here’s where you come in! (For more on cost, see the below video clip.)
Lymphedema Treatment Act (LTA)
The Lymphedema Treatment Act was passed in December of 2022. But the legislation details are still being worked out. Heather Ferguson is the founder of this legislation. She sends out a newsletter with updates. And she needs your help. Please read the below letter, & contact your insurance company. Heather makes it easy for you by providing templates & links.
LETTER: https://ltstherapy.com/wp-content/uploads/2023/09/LTA-1.pdf
Action Item #1: click here
Action Item #2: click here
References
1 Foldi, M, Foldi, E. (2006). Foldi’s Textbook of Lymphology (2nd ed.), p. 595. Germany: Urban and Fisher. Foldi, M., & Foldi, E. (2012). Foldi’s Textbook of Lymphology (3rd ed.). Urban and Fisher.