Last month, we discussed phase I (decongestion therapy) in lymphedema treatment. This month, we’ll pick up with phase II & also discuss adjuncts. If you’ve got lymphedema & made a New Year’s resolution, this post may help.
Phase II: Lymphedema Maintenance
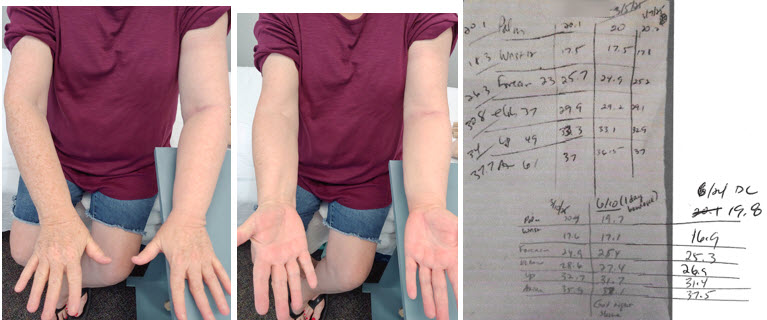
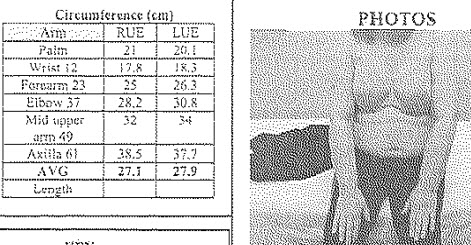
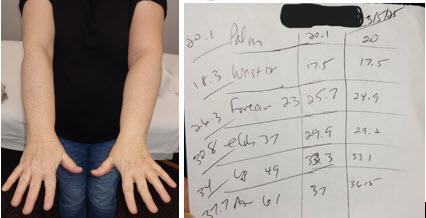
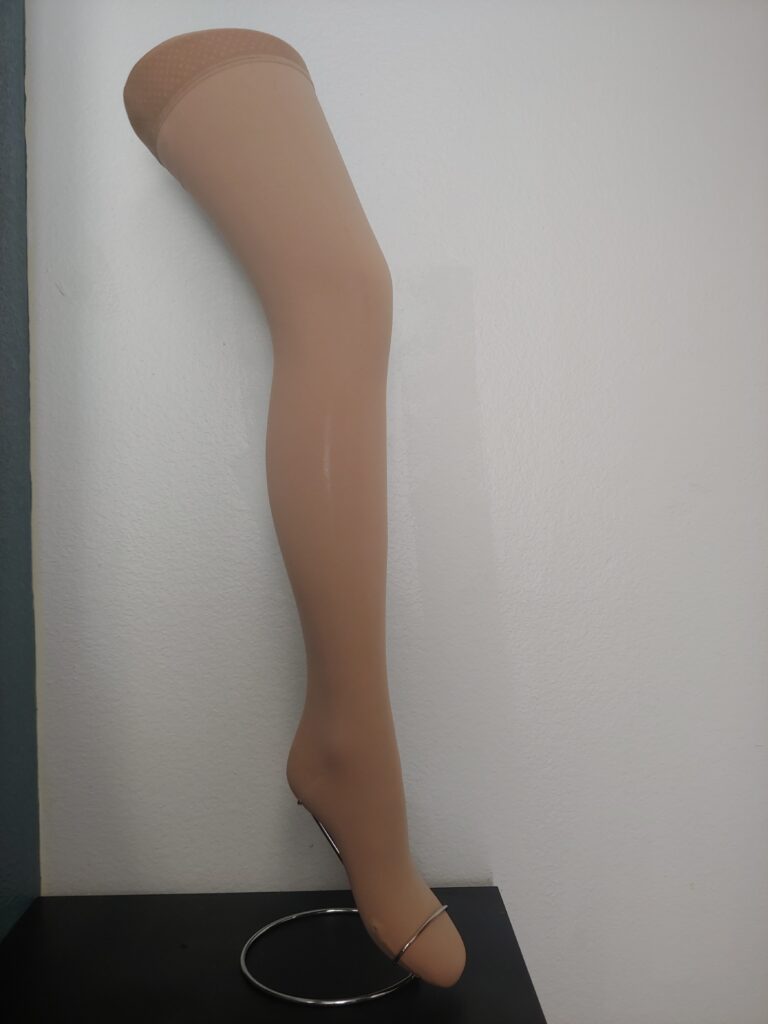
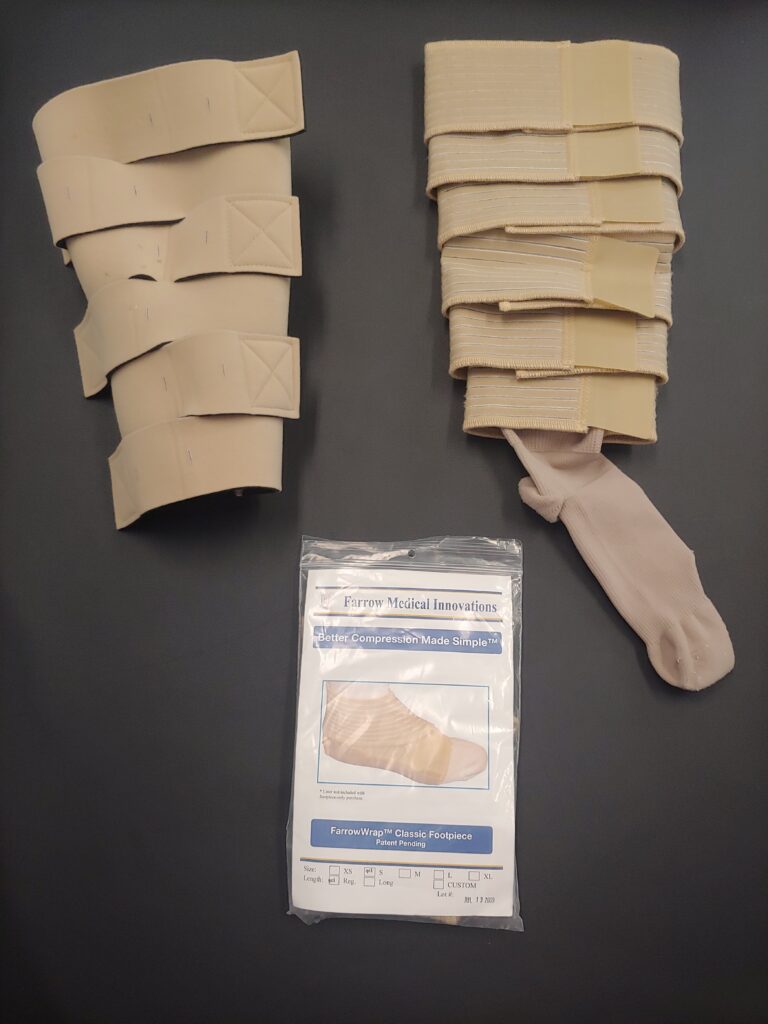
Assuming a patient is compliant with guidelines, they should progress to phase II fairly predictably (the maintenance phase). This begins immediately after phase I & involves being fit with a compression garment to maintain the volume loss & fibrosis reduction attained in phase I. Sometimes the garment doesn’t fit quite right in the first try. So, a revised garment must be ordered. In my experience, patients frequently try to short cut this phase, too, by:
- wearing elastic garments (off the shelf, circular-knit garments) instead of resuming bandaging while waiting for the revised garment
- wearing the garment to be returned (which is improperly fit)
- not wearing a night garment or using an inappropriate night garment.
These decisions can cause refilling & regression.
As noted earlier, if a person begins phase I in stage II or III lymphedema, fibrosis is likely still going to be present to some extent at the end of treatment. But it should continue to gradually reduce in phase II with the appropriate compression & compliance.7
Phase II is generally “maintenance for life.”9 In my experience, when a person is compliant & sticks to the above protocol, phase II will maintain their lymphedema. And, lymphedema can continue to improve. However, people often, again, try shortcuts (i.e. no night garment, noncompliance with daily use of their daytime garment, etc.). On occasion, particularly if a person is in stage II or III lymphedema (or if they took shortcuts or have not been compliant), they may need to resume intensive phase I treatment in the future.
Phase II Adjuncts
There are several adjuncts to lymphedema maintenance. We just talked about one the past two blog posts. “Adjunct” means “supplement” or “auxiliary function,” not a standalone or essential role. In other words, these aren’t necessary components to maintenance. But some people may find some beneficial effects.

A chameleon appears to be one thing but is actually another. Like a chameleon, certain adjunct therapies may be seem to be a “cure” for lymphedema, but they may not be what they appear.
The following are examples of adjuncts for lymphedema.
- Compression pumps10, 18
- Medications: Flavonoids, benzopyrones11 & synbiotics18
- Aquatics12, 18 – compression applied by water during exercise
- Ultrasound13, 18 – uses sound waves to cause vibrations which may help with fibrosis but it can create friction & heat (which increases fluid creation).**
- Hivamat13, 18 -uses an electrostatic field to create a deep, gentle oscillation in the tissue, which helps reduce fibrosis, inflammation & improve lymphatic flow
- Rebounders16 – trampolines require you to use your muscles. As encouraged by any exercise, muscle contraction impacts lymphatic function by squeezing lymph vessels, which helps to propel lymph fluid through the body. While contraction increases interstitial fluid pressure and can compress vessels, the relaxation phase is crucial for allowing fluid to enter the lymphatics. Exercise causes an increase in blood flow (increasing fluid in the tissue spaces). Compression garments counteract this process by providing working pressure that promotes lymph fluid removal from the tissue space. So, it’s important to wear compression during any exercise to prevent refilling & to aid in the uptake of fluid in the lymphatic vessels.
- Vibration14, 18 – stimulates the lymphatic system by causing rapid muscle contractions that help pump lymph fluid through the vessels. As with any exercise, it’s important to wear compression during use.
- Diet17 – despite books & social media posts, there is no “lymphedema diet.” Nothing you eat is going to cure lymphedema. However, eating a poor diet & gaining weight can exacerbate lymphedema. Salt, sugar & alcohol consumption can negatively impact water retention & inflammation, thus exacerbating lymphedema.
- Kinesio taping18 (elastic taping) may facilitate lymphatic drainage
- Photobiomodulation (low-level laser)18 – red light therapy & near-infrared light can stimulate cellular function, reduce inflammation & enhance lymphangiogenesis & lymphatic motility
- Extracorporeal shock wave therapy (ESWT)18 – a noninvasive treatment that uses acoustic shock waves to reduce fibrosis & enhance lymphangiogenesis (new lymphatic vessel growth).
- Acupuncture and Moxibustion18** Acupuncture works by inserting fine needles into specific points on the body (up to two inches deep into skin) to stimulate biochemical reactions, while moxibustion uses heat from burning mugwort to warm acupuncture points.
- Negative pressure (cupping)18** – creates suction, drawing the skin and tissue upward. This suction increases blood flow. It can also cause skin redness & discoloration that persists for some time after the procedure. According to Foldi, manual lymph drainage should be gentle & light in pressure (pressure sufficient to stretch the skin, not heavy enough to cause redness). This is because the lymph vessels are less than one millimeter in diameter on average with more superficial vessels being even smaller. (As a reference, 1 millimeter = 0.03937 inches.) If too much force is used in MLD (or otherwise), the delicate anchoring filaments can be injured or deeper lymphangions can go into spasm.”20 Note: MLD force and compression-garment pressure behave completely differently physiologically and mechanically, even though both affect lymph flow. MLD involves directional shear, not uniform compression. That’s why pressure must be extremely low. Compression garments apply broad, evenly distributed, static external pressure across the entire limb (not directional shear).
Personally, I would avoid the above adjuncts marked with an asterisks as they cause hyperemia (an increase in blood flow) which increases lymphatic load & could exacerbate lymphedema. The exception is activities in which you have or use compression (such as aquatics or exercise). In Foldi’s words, “[a]t a minimum, methods that result in hyperemia should be avoided wherever possible.19, 20
References
1 Foldi, M, Foldi, E. (2006). Foldi’s Textbook of Lymphology (2nd ed.), p. 273. Germany: Urban and Fisher.
2 Foldi, M, Foldi, E. (2006). Foldi’s Textbook of Lymphology (2nd ed.), p. 245, 322. Germany: Urban and Fisher.
3 Foldi, M, Foldi, E. (2006). Foldi’s Textbook of Lymphology (2nd ed.), p. 246. Germany: Urban and Fisher.
4 Foldi, M, Foldi, E. (2006). Foldi’s Textbook of Lymphology (2nd ed.), p. 272. Germany: Urban and Fisher.
5 Foldi, M, Foldi, E. (2006). Foldi’s Textbook of Lymphology (2nd ed.), p. 281. Germany: Urban and Fisher.
6 Adjuncts – Foldi, M, Foldi, E. (2006). Foldi’s Textbook of Lymphology (2nd ed.), p. 282. Germany: Urban and Fisher.
7 Fibrosis – Foldi, M, Foldi, E. (2006). Foldi’s Textbook of Lymphology (2nd ed.), p. 273-274. Germany: Urban and Fisher.
8 Inpatient – Foldi, M, Foldi, E. (2006). Foldi’s Textbook of Lymphology (2nd ed.), p. 273. Germany: Urban and Fisher.
9 For life – Foldi, M, Foldi, E. (2006). Foldi’s Textbook of Lymphology (2nd ed.), p. 274. Germany: Urban and Fisher.
10 Pumps – Foldi, M, Foldi, E. (2006). Foldi’s Textbook of Lymphology (2nd ed.), p. 283. Germany: Urban and Fisher.
11 Meds – Foldi, M, Foldi, E. (2006). Foldi’s Textbook of Lymphology (2nd ed.), p. 283. Germany: Urban and Fisher.
12 Aquatics – Foldi, M, Foldi, E. (2006). Foldi’s Textbook of Lymphology (2nd ed.), p. 559 Germany: Urban and Fisher.
13 Ultrasound & Hivamat – Foldi, M, Foldi, E. (2006). Foldi’s Textbook of Lymphology (2nd ed.), p. 560. Germany: Urban and Fisher.
14 Vibration – Rauch F, Sievanen H, Boonen S, et al. Whole-body vibration and blood flow and muscle oxygenation: a meta-analysis. Clin Physiol Funct Imaging. 2015;35(2):97–104. (This meta-analysis shows that whole-body vibration (WBV) increases peripheral blood flow — a mechanism potentially relevant to lymphatic drainage.)// Casarotto RA, Tonezzer T, Munaretto Timm Baiocchi J, Harari D. Effects of the vibratory platform on the treatment of lymphedema post-breast cancer surgery: case studies. World Physiotherapy Congress Proceedings. 2022.
15 RLT – Carati CJ, Anderson SN, Gannon BJ, Piller NB. Treatment of postmastectomy lymphedema with low-level laser therapy: a double-blind, placebo-controlled trial. Cancer. 2003;98(6):1114–1122. // Ridner SH, Poage-Hooper E, Kanar C, Doersam JK, Bond SM, Dietrich MS. A pilot randomized trial evaluating low-level laser therapy as an alternative treatment to manual lymphatic drainage for breast cancer–related lymphedema. Oncol Nurs Forum. 2013;40(4):383–393. // Li K, Zhang Z, Liu NF, Feng SQ, Tong Y, Zhang JF, et al. Efficacy and safety of far infrared radiation in lymphedema treatment: clinical evaluation and laboratory analysis. Lasers Med Sci. 2017;32(3):485–494. // Ueno N, Fukuzawa H, Oshima T, et al. Far infrared radiation therapy for gynecological cancer–related lymphedema is an effective and oncologically safe treatment: a randomized-controlled trial. Lymphology. 2021;54(3):141–150.
16 Rebounders – https://www.thecancerspecialist.com/2019/08/01/the-benefits-of-rebounding-in-the-prevention-and-management-of-lymphedema/
17 Diet – Foldi, M, Foldi, E. (2006). Foldi’s Textbook of Lymphology (2nd ed.), p. 269, 305. Germany: Urban and Fisher.
18 https://lymphnet.org/page/position-papers (National Lymphedema Network Position Paper on maintenance)
19 Foldi, M, Foldi, E. (2006). Foldi’s Textbook of Lymphology (2nd ed.), p. 559. Germany: Urban and Fisher.
20 Foldi, M, Foldi, E. (2006). Foldi’s Textbook of Lymphology (2nd ed.), p. 526. Germany: Urban and Fisher.