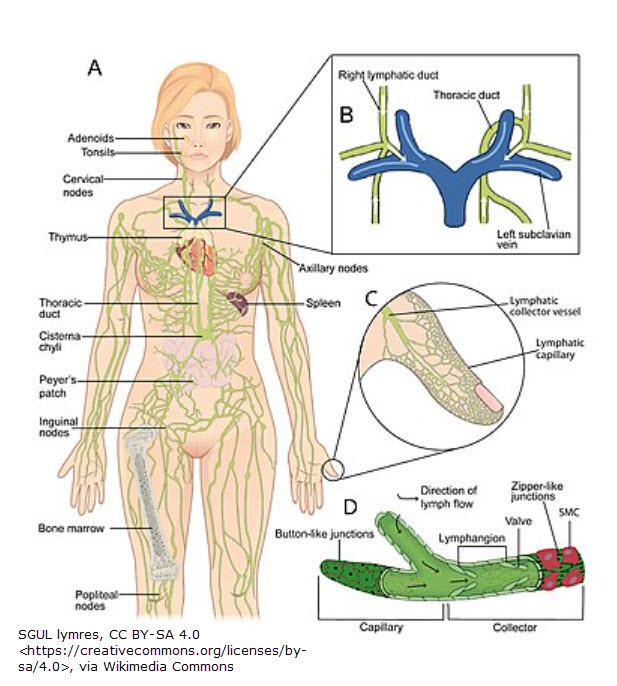
As you know from last month’s blog, the Lymphedema Treatment Act (LTA) was passed in December of 2022. Most of 2023 has been spent with Heather Ferguson & others communicating with legislators & Medicare on what should be included in the bill coverage.
Bill Coverage
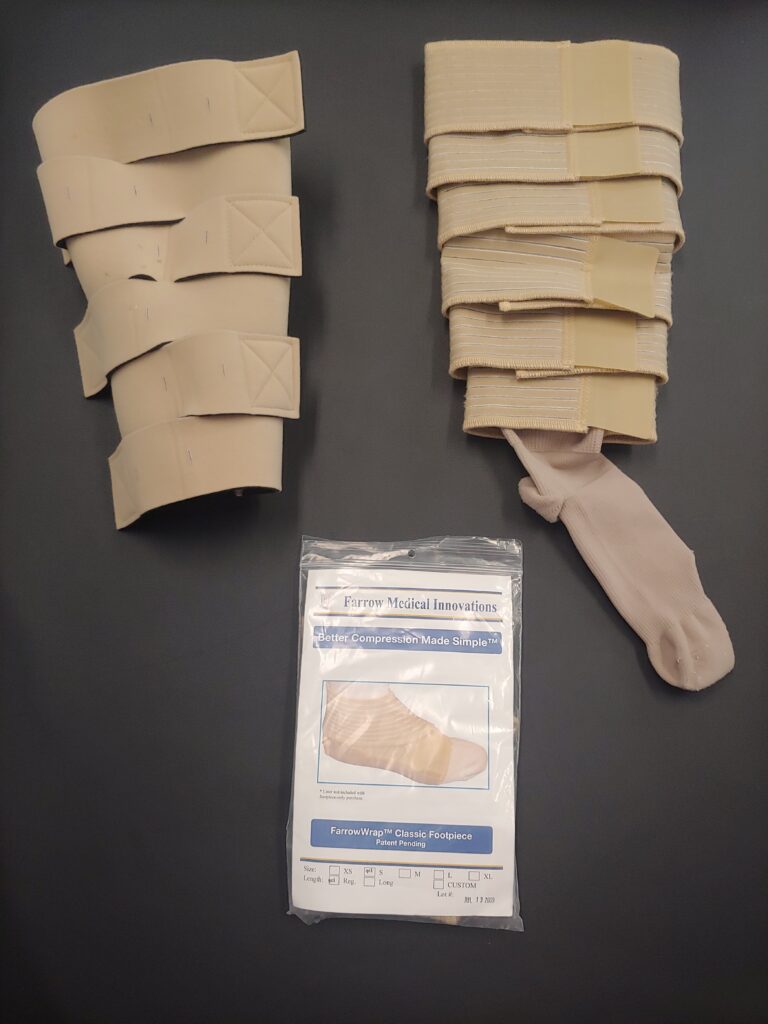
On page 45 of the “Medicare and You 2024” handbook,1 it states if you have a diagnosis of lymphedema, Medicare will cover your medically gradient compression garments (with a physician’s prescription) at 80%. Coverage is for standard, off-the-shelf garments or custom-fitted garments. You’ll pay your 20% (unless you have a supplemental plan). Your part B deductible applies.
The proposed final rule is a more specific.2 It states medically gradient compression garments (readymade or custom, Velcro or other) will be covered as well as bandaging supplies. Anyone providing these items must be enrolled with Medicare as a DME supplier & meet supplier standard requirements.
Where You Can Find a Supplier Who Can Bill For Compression Garments
You can use Medicare’s online search tool3 to search for a supplier capable of billing for the items. One concern I have is whether these will be competent fitters (vs standard DME suppliers whose knowledge is typically limited to basic sleeves & hose). Lymphedema Therapy Source plans to use a second business to bill for lymphedema supplies & compression (including pneumatic compression pumps). This will include a lengthy process of becoming an enrolled DMEPOS supplier, becoming accredited, meeting all DME supplier and quality standards, obtaining a surety bond & submitting claims to the appropriate Medicare contractor for DME. (No small task!)
Billing Codes4 (see updates at the end of page)
While therapy services are billed using CPT codes, products (or DME supplies) are billed with HCPCS Level II codes. Below is a list of expected codes & descriptions for lymphedema compression items covered by Medicare as a result of the Lymphedema Treatment Act.
HCPCS Codes for Compression Treatment Items:
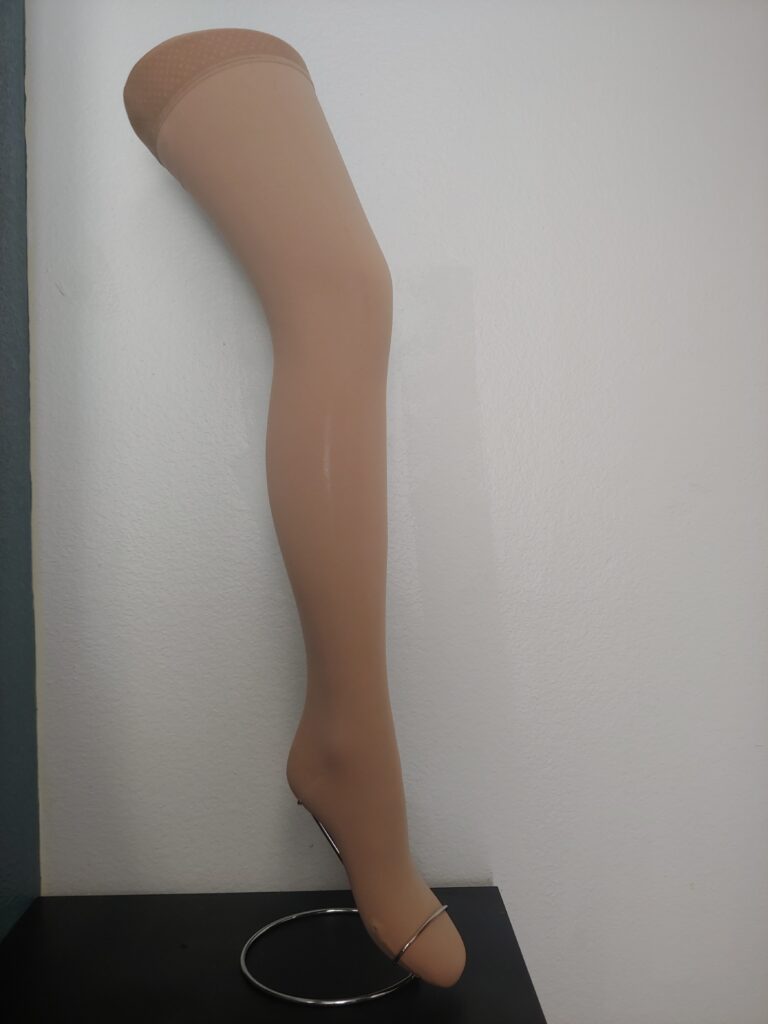
Compression Hose
A6530 Gradient compression stocking, below knee, 18-30 mmHg each
A6531 Gradient compression stocking, below knee, 30-40 mmHg, each*
A6532 Gradient compression stocking, below knee, 40-50 mmHg, each*
A6533 Gradient compression stocking, thigh length, 18-30 mmHg, each
A6534 Gradient compression stocking, thigh length, 30-40 mmHg, each
A6535 Gradient compression stocking, thigh length, 40-50 mmHg, each
A6536 Gradient compression stocking, full length/chap style, 18-30 mmHg, each
A6537 Gradient compression stocking, full length/chap style, 30-40 mmHg, each
A6538 Gradient compression stocking, full length/chap style, 40-50 mmHg, each
A6539 Gradient compression stocking, waist length, 18-30 mmHg, each
A6540 Gradient compression stocking, waist length, 30-40 mmHg, each
A6541 Gradient compression stocking, waist length, 40-50 mmHg, each
Velcro (or other)
A6545 Gradient compression wrap, non-elastic, below knee, 30-50 mmHg, each*
A6549 Gradient compression stocking/sleeve, not otherwise specified
Compression Sleeves & Gloves
S8420 Gradient pressure aid (sleeve and glove combination), custom made
S8421 Gradient pressure aid (sleeve and glove combination), readymade
S8422 Gradient pressure aid (sleeve), custom made, medium -weight
S8423 Gradient pressure aid (sleeve), custom made, heavy -weight
S8424 Gradient pressure aid (sleeve), readymade
S8425 Gradient pressure aid (glove), custom made, medium -weight
S8426 Gradient pressure aid (glove), custom made, heavy -weight
S8427 Gradient pressure aid (glove), readymade
S8428 Gradient pressure aid (gauntlet), readymade
Other (including treatment supplies)
S8429 Gradient pressure exterior wrap
S8430 Padding for compression bandage, roll
S8431 Compression bandage, roll
There may be changes to some of these codes. For those with an asterisks (*), new HCPCS codes may be assigned when these items are used as surgical dressings (such as in the case of an open venous stasis ulcer).
***UPDATE 11/30/23***
Beginning in 2024, there will be 81 HCPSC codes specifically for lymphedema compression supplies (most will be new).
Where You Can Find More Information
Visit the Lymphedema Treatment Act for more information & an up-to-date status on the bill & its coverage: https://lymphedematreatmentact.org/faqs/.
A special thank-you to Heather Ferguson & her team for their ongoing fight to get the LTA passed.
***UPDATE 01/05/24***
Lymphedema HCPCS billing codes have been published & are listed here. A person must have one of the following diagnosis codes:
- I89.0 (lymphedema, not elsehwere classified)
- I97.2 (postmastectomy lymphedema)
- I97.89 (Other postprocedural complications and disorders of the circulatory system, not elsewhere classified)
- Q82.0 (hereditary/primary lymphedema)
References
1 https://www.medicare.gov/publications/10050-Medicare-and-You.pdf
2 https://lymphedematreatmentact.org/wp-content/uploads/2023/07/LTA-Section-Home-Health-Rule.pdf
3 https://www.medicare.gov/medical-equipment-suppliers/
4 LTA Home Health Rule, p. 13