Reason 2 – Inadequate Treatment
In part 1, we looked at one reason CDT may not work. In part 2, we’ll look at the important components of lymphedema treatment.
Complete Decongestive Therapy (CDT) involves (4) pillars of treatment:
1. Manual lymph drainage (MLD)
2. Multilayer compression bandaging
3. Skin Care
4. Exercise
If one of these is lacking (particularly 1, 2 & 4), a patient will not maximize their potential. Let’s look at each of these individually.

Manual Lymph Drainage
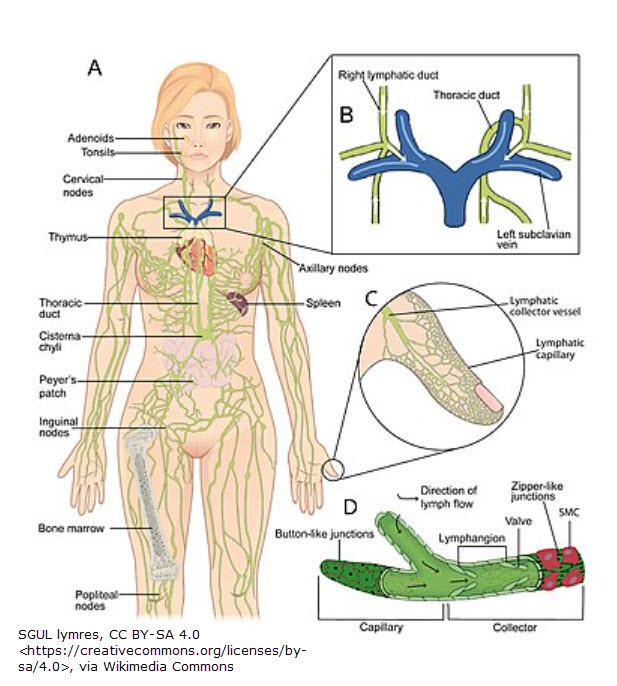
The purpose of MLD is to remove the protein in the interstitial tissue space. (The protein accumulation is due to damage of the lymphatic system – from a birth defect or a secondary cause.) Bandaging without MLD might squeeze the “water” from the tissue space, but it won’t remove the protein (neither will diuretics). That’s a specific function of MLD. And if protein attracts water, what will the result be? More swelling.
I’ve recently read & heard that there isn’t proof that MLD works. But there is research to back the efficacy of MLD.
- In a 2017 study published in the Lymphatic Research and Biology Journal, near-infrared imaging was used to track a dye (indocyanine green) in nine healthy participants before & after a 15-minute period of MLD followed by a compression garment for 10 minutes applied to the arm. Images were taken at the forearm & elbow. There was a statistically significant improvement in the movement of lymph fluid & the speed of transport. At baseline, lymph transport speed was 6.7 millimeters per second (mm/s). This increased to 13.3 mm/s after MLD! Speed increased by 10.5 mm/s after use of a compression garment.3
- Another study published in 2011 also used near-infrared imaging to assess the speed of lymph contractile function before & after MLD. Results showed lymph transport speed increased by 23% in symptomatic limbs (ones with lymphedema) & 25% in asymptomatic limbs (ones without lymphedema).4
Characteristics of MLD include a gentle, 2-way stretch of the skin (approximately 1 stretch per second8) that create a “pulling & shear force.”12 If too much pressure is applied, anchoring filaments of the initial lymphatic vessels close to the skin’s surface may be damaged. If MLD strokes are performed too fast or too firm, lymphangions may spasm.8 Frequency of MLD should be daily in Phase I (the decongestion phase).1 If MLD is not administered correctly or with less frequency than recommended, results will show it.
Multilayer compression bandaging
Compression is an essential part of CDT. According to Foldi’s Textbook,1 a study from the European Journal of Cancer assessed the outcome of MLD in breast cancer-related lymphedema. The study found that MLD reduces limb volume & dermal (skin) thickness in the upper arm.5 In contrast, the 9th edition of the Munich Cancer Center manual reported a deterioration in arms of women with lymphedema who received lymph drainage but did not wear compression sleeves.
The International Lymphoedema Framework publishes a best practice guideline for compression.6 The upper body guideline states, “The application of a compression garment results in constant pressure on the skin when the limb is at rest (resting pressure). When the muscles contract, expand and then relax (e.g. during exercise), they transiently press against the resisting garment and so the tissue pressure in the limb increases temporarily.” This pressure increase “compresses the adjacent dermal lymphatics and because the collecting and larger lymphatics are valved, these vessels pump passively so that lymph flows up the arm without the lymphatics having to contract.” In other words, the resistance provided by compression increases tissue pressure &, as a result, lymph movement.
Other benefits of compression include softening of fibrotic tissue & improving the venous pump function.10 Foldi states, “In lymphedema, one should always use the maximum compression that is tolerated by the patient.”7 (A 2016 study found 84 mmHg compression stopped lymphatic flow.8 This is extremely high pressure. Compression seldom goes above ~46 mmHg in lymphedema garments & limb size should be considered. Smaller circumferences like fingers & arms will not tolerate the same compression that legs might.)
Compression is an important component of CDT. If it is lacking in the treatment phase or maintenance phase, there will not be sufficient volume reduction or containment. If compression bandages are removed between sessions, refilling will occur. And if bandages are not applied correctly, there can be adverse consequences such as increased swelling or pressure wounds.
Skin Care
Good hygiene & using acidic products more like the skin’s natural pH level will reduce itching & improve skin texture. These will also help mitigate potential infections due to a compromised skin barrier.
Exercise
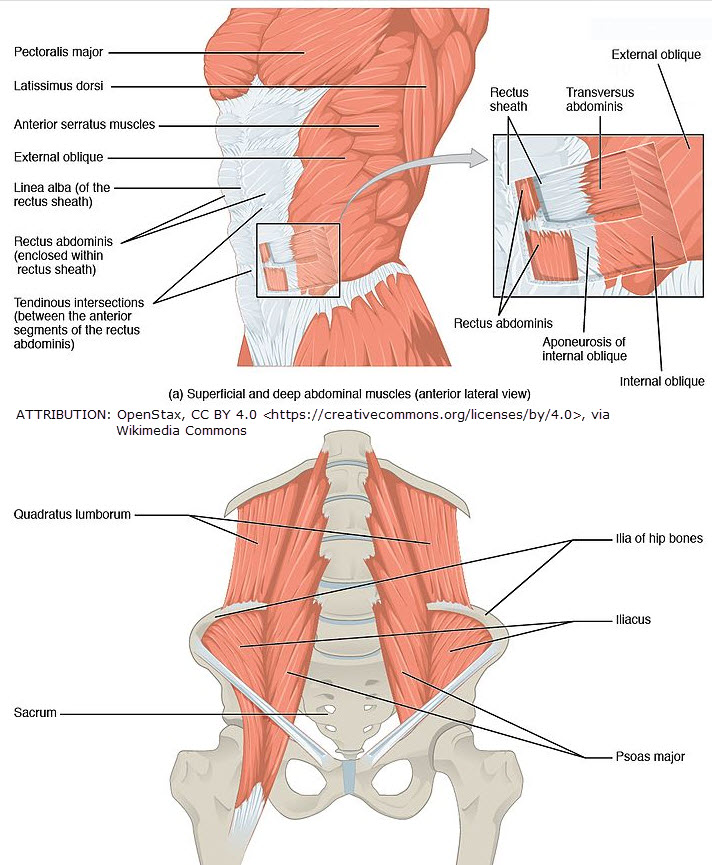
When the body is at rest, only a minor amount of lymph is formed.12 Movement is key to lymph creation. Exercise engages the muscle pump. Singing, deep breathing & laughing are excellent ways to engage the diaphragm & compress the most important lymph vessel in the body (the thoracic duct).11 Exercising with compression increases tissue pressure (& so lymph movement) & softens fibrosis in extremities (helping to reduce volume).
In summary, all aspects of CDT are important components. If one is overlooked or administered inadequately, CDT may fail at worst or results may be subpar at best.
References
1 Foldi, M, Foldi, E. (2006). Foldi’s Textbook of Lymphology (2nd ed.), p. 272. Germany: Urban and Fisher. Foldi, M., & Foldi, E. (2012). Foldi’s Textbook of Lymphology (3rd ed.). Urban and Fisher.
2 https://www.lympho.org/publications
3 Lopera C, Worsley PR, Bader DL, Fenlon D. Investigating the Short-Term Effects of Manual Lymphatic Drainage and Compression Garment Therapies on Lymphatic Function Using Near-Infrared Imaging. Lymphat Res Biol. 2017;15(3):235-240. doi:10.1089/lrb.2017.0001
4 Tan IC, Maus EA, Rasmussen JC, et al. Assessment of lymphatic contractile function after manual lymphatic drainage using near-infrared fluorescence imaging. Arch Phys Med Rehabil. 2011;92(5):756-764.e1. doi:10.1016/j.apmr.2010.12.027
5 Williams AF, Vadgama A, Franks PJ, Mortimer PS. A randomized controlled crossover study of manual lymphatic drainage therapy in women with breast cancer-related lymphoedema. Eur J Cancer Care (Engl). 2002;11(4):254-261. doi:10.1046/j.1365-2354.2002.00312.x
6 Moffatt, CJ, et al. International Lymphedema Framework. (p. 13)
7 Foldi, M, Foldi, E. (2006). Foldi’s Textbook of Lymphology (2nd ed.), p. 273. Germany: Urban and Fisher. Foldi, M., & Foldi, E. (2012). Foldi’s Textbook of Lymphology (3rd ed.). Urban and Fisher.
8 Foldi, M, Foldi, E. (2006). Foldi’s Textbook of Lymphology (2nd ed.), p. 526. Germany: Urban and Fisher. Foldi, M., & Foldi, E. (2012). Foldi’s Textbook of Lymphology (3rd ed.). Urban and Fisher.
9 Belgrado JP, Vandermeeren L, Vankerckhove S, et al. Near-Infrared Fluorescence Lymphatic Imaging to Reconsider Occlusion Pressure of Superficial Lymphatic Collectors in Upper Extremities of Healthy Volunteers. Lymphat Res Biol. 2016;14(2):70-77. doi:10.1089/lrb.2015.0040
10 Foldi, M, Foldi, E. (2006). Foldi’s Textbook of Lymphology (2nd ed.), p. 568-569. Germany: Urban and Fisher. Foldi, M., & Foldi, E. (2012). Foldi’s Textbook of Lymphology (3rd ed.). Urban and Fisher.
11 Shields, J. (1992). Lymphology, v25, n4, Dec. 1992, p. 147* & Foldi, M, Foldi, E. (2006). Foldi’s Textbook of Lymphology (2nd ed.), p. 550. Germany: Urban and Fisher. Foldi, M., & Foldi, E. (2012). Foldi’s Textbook of Lymphology (3rd ed.). Urban and Fisher.
12 Foldi, M, Foldi, E. (2006). Foldi’s Textbook of Lymphology (2nd ed.), p. 198. Germany: Urban and Fisher. Foldi, M., & Foldi, E. (2012). Foldi’s Textbook of Lymphology (3rd ed.). Urban and Fisher.
* https://lymphaticyoga.net/deep-breathing-and-the-lymphatic-system/ cites Dr. Shields as saying, “Deep diaphragmatic breathing stimulates the cleansing of the lymph system by creating a vacuum effect which pulls the lymph through the bloodstream.” I cannot find this statement in the cited article posted by the author. (https://journals.uair.arizona.edu/index.php/lymph/article/view/17643/17366)