Last month, we looked at what happens during a woman’s period. This month, we’ll talk about how MLD can help.
Symptoms MLD May Help
In the second half of a cycle (the luteal phase), all kinds of unwelcomed symptoms can emerge. These can include bloating, cramps, weight gain, mood swings, fatigue, constipation, headaches & food cravings. These symptoms are caused by the rise & sudden, sharp drop of progesterone (& estrogen) when there is no egg fertilization (i.e. pregnancy). This hormone shift can affect brain chemistry, especially serotonin, which influences mood and emotion.
- Bloating & Water Retention – Progesterone affects fluid balance by acting on the kidneys and blood vessels. Its drop can cause fluid to accumulate, leading to bloating, breast tenderness, and mild weight gain.
- Cramps (Dysmenorrhea) – As hormone levels fall, the body produces prostaglandins to help shed the uterine lining. These chemicals cause the uterus to contract, which can lead to pain and cramping. Higher prostaglandin levels = more intense cramps.
- Constipation – High progesterone (& estrogen) slows down smooth muscle contractions in the digestive tract (motility). This can lead to slower digestion and constipation, especially in the days following ovulation.
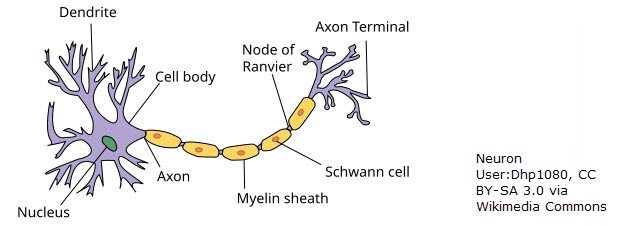
- Headaches – Estrogen influences how blood vessels expand and contract and affects neurotransmitters like serotonin. When estrogen drops, it can trigger headaches or migraines, especially in those sensitive to hormonal changes.
- Fatigue – The body goes through energy-intensive changes during the luteal phase, and the falling hormones can also impact thyroid function and serotonin, leading to tiredness or sleep disruption.
- Food Cravings – Estrogen and progesterone influence insulin sensitivity and appetite-regulating neurotransmitters like dopamine and serotonin. The drop can cause cravings (especially for sugar and carbs), which temporarily boost serotonin and make you feel better — at least short-term.
- Mood Swings & Irritability – Estrogen and progesterone affect brain chemistry, including: Serotonin (mood), GABA (calmness and anxiety) & Dopamine (pleasure and motivation). When these hormones drop, serotonin levels can dip, contributing to irritability, anxiety, sadness, or mood swings. Sensitivity to this drop varies. Some women experience mild PMS while others experience more severe PMS.
How MLD May Help
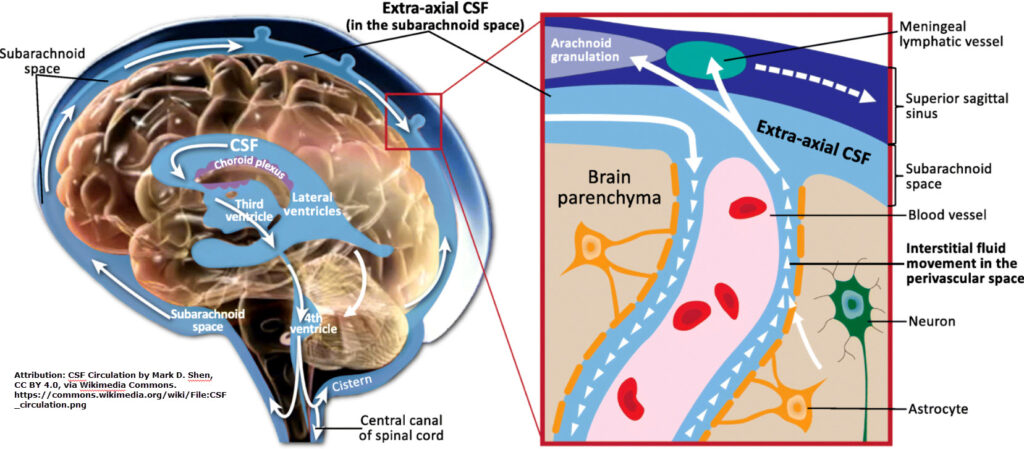
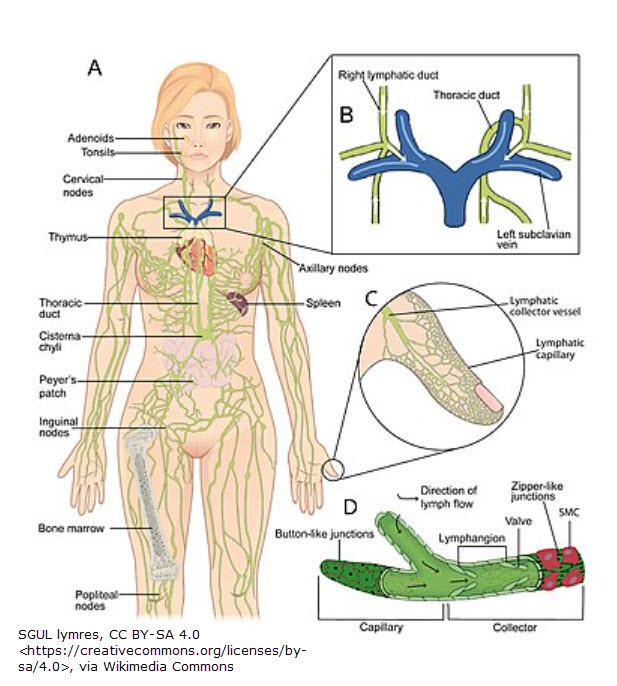
MLD increases lymphangiomotion (lymph pumping). By doing so, inflammatory particles & excess fluid are removed. In addition, proper MLD has a very relaxing effect on the body. So, it could help mood. Unfortunately, I’m not aware of any impact on food cravings!
- Bloating and Water Retention – MLD gently stimulates the lymphatic system, which is responsible for removing excess fluid and waste from tissues. By improving lymph flow, it can reduce puffiness, bloating, and that heavy, swollen feeling often reported in the days before menstruation.
- Breast Tenderness – Swollen, tender breasts are often caused by fluid buildup and hormonal shifts. MLD around the neck, armpits, and chest area can reduce this fluid accumulation and ease discomfort.
- Headaches (from fluid pressure) – If headaches are partially due to congestion in the head and neck, MLD may help by encouraging drainage and reducing pressure.
- Fatigue (mild benefit) – Some women report feeling more energized after MLD, likely due to improved circulation and detoxification, though this effect varies from person to person.
- Constipation – After ovulation, progesterone levels rise before dropping. During this rise, progesterone has a relaxing effect on smooth muscle, including the muscles of the gastrointestinal (GI) tract. This causes slower gut motility (i.e. food moves more slowly through the intestines) which can lead to harder stools, less frequent bowel movements and bloating and gas. Gentle abdominal MLD techniques may improve circulation of lymphatic fluid around the intestines and abdominal organs, reducing congestion, inflammation, or sluggish movement. It can also help reduce fluid retention and bloating in the abdomen, which can make constipation feel worse. With less abdominal pressure, the bowel may move more freely.3
- Mood – While MLD may not directly affect mood, it can help with reducing stress and tension, which may indirectly support better mood regulation & feelings of well-being.
Caution
MLD is not a standalone treatment for PMS. It works best when combined with hydration, fiber, movement, and sometimes probiotics or dietary adjustments. Pending a doctor’s approval, NSAIDS like Ibuprofen or heating pads may be helpful for severe cramps. And, in some cases, birth control pills can help regulate a cycle & improve symptoms. With any medication, it’s important to be aware of side effects. And be aware that deep abdominal techniques are contraindicated during menses.
Cycle Idiopathic Edema
While talking about PMS, it’s a good idea to mention another condition: Idiopathic cyclic edema (ICE). ICE is a condition that resembles PMS but is different. Besides similar symptoms, women often have two good weeks followed by two bad weeks of swelling. Oddly, even though considered edema, it is a protein-rich fluid. So, MLD & compression can be helpful.1 It mostly affects women & causes daily, unpredictable swelling, especially in the legs, hands, face, and sometimes abdomen, with no identifiable underlying disease. (The term “idiopathic” means the exact cause is unknown, and “cyclic” refers to the pattern of swelling that comes and goes, often worsening throughout the day.) Although the cause is not clear, a number of hormones (particularly the luteinizing hormone)1 are postulated to be involved. Altered vascular permeability and increased lymph formation may also be part of the disorder.2
References
1 Kasseroller, R. (1998). Compendium of Dr. Vodder’s Manual Lymph Drainage, pg.111. Germany: Huthig GmbH.
2 Sabatini S. Hormonal insights into the pathogenesis of cyclic idiopathic edema. Semin Nephrol. 2001;21(3):244-250. doi:10.1053/snep.2001.21651
3 Wittlinger, H., Wittlinger, G. (1998). Textbook of Dr. Vodder’s Manual Lymph Drainage (6th ed.), pg. 87. Germany: Karl Haug Verlag.