This month’s blog is dedicated to advocacy for providers.
Most people dealing with lymphedema aren’t aware of the behind-the-scenes challenges providers face when it comes to providing care. The administrative burden to small practices like mine is immense.
Lymphedema Treatment Act
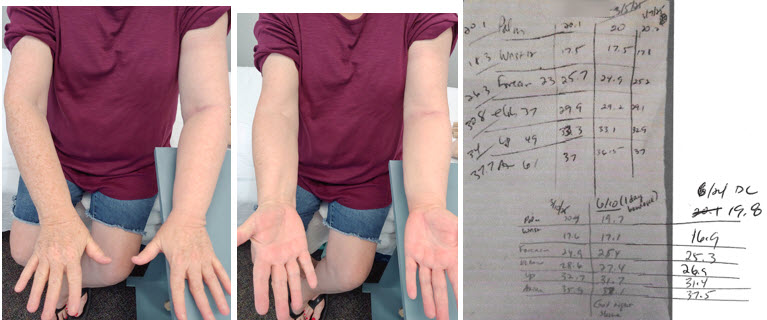
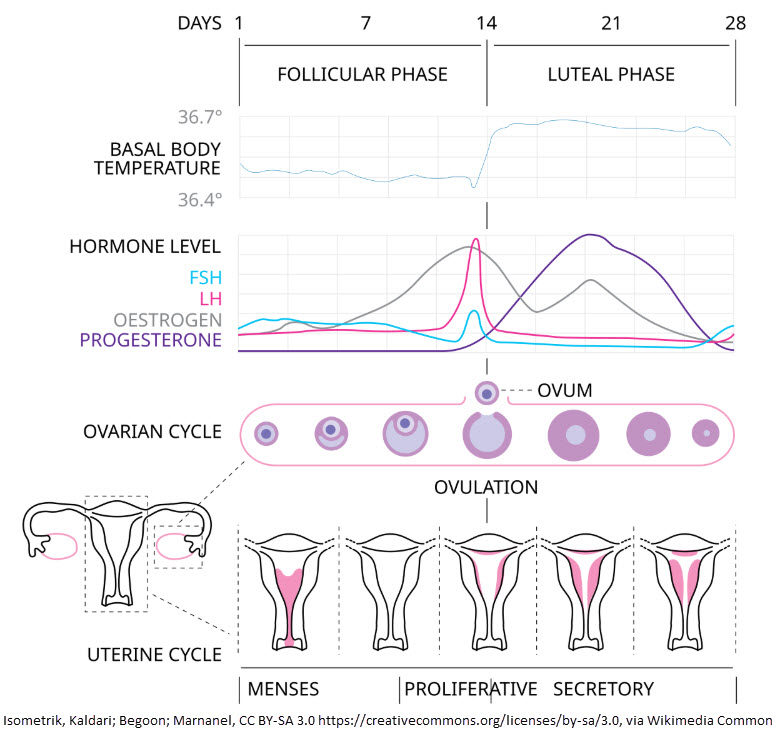
In past blogs, I’ve brought attention to the Lymphedema Treatment Act (LTA) in blog posts: Oct-Dec 2023 & Feb-March 2024. After over a decade of struggles, the LTA was finally passed. As a result, Medicare now pays for lymphedema compression & treatment supplies. (Such costs were a huge barrier for many patients.) This time, I’m bringing attention to a related topic impacting providers.
Provider Impact
When patients are looking for providers, they generally seek providers in-network (providers who contract with their insurance plan to accept payment as opposed to out of network providers who may accept their insurance plan but don’t accept their payment as payment in full). Finding an in-network provider means lower cost for the patient. But it also means lower payment to the provider. In addition, providers are always paid for all services provided. While this may not be an immediate concern for patients who don’t feel the financial burden, it will be a concern in the long run as fewer providers opt to contract directly with insurers for in-network status — in a field in which there are already few qualified, trained lymphedema practitioners.
The good news is that just like with lymphedema legislation, there are avenues for change. This blog is an example of what providers (& patients) can do. In an age of technology in which Ai can do all the “heavy lifting,” there’s no excuse for not taking action. Such an opportunity presented itself this month.
Providers can experience burnout from patient care. This can be magnified by administrative burdens & reduced payments.

Reduced Payments
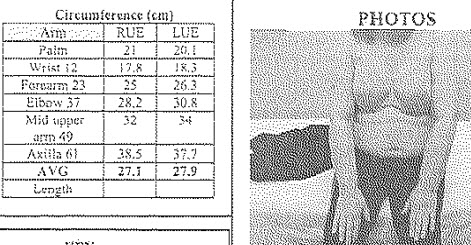
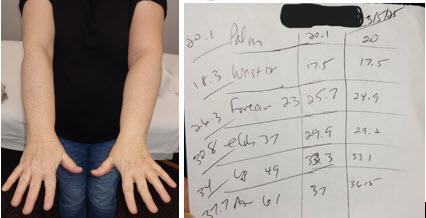
My business contracts with numerous plans by insurers like Medicare, BCBS, Cigna (via American Specialty Network or ASH through which therapists must contract) & United Healthcare. My fee schedule is based off Medicare’s fee schedule. While a very few pay more, most insurers pay less, & more commonly they further reduce payment by not paying for certain services when done in the same session (such as CPT codes 97535 training & 29581 bandaging, or 97140 massage & 29581 bandaging). They consider these to be bundled services. However, they are often separate services which can standalone & are a necessary part of care. For example, manual lymph drainage (97140) & bandaging (29581 / 29584) are a part of nearly every lymphedema treatment session during the decongestion phase.
Added Fees
When insurance companies pay a provider for service, they often have “processing fees.” This fee is a percentage of what they pay you. (Providers already get charged a processing fee for accepting your payment via card – if they don’t pass it on to you.) American Specialty Network (a.k.a. “ASH” – contractor for Cigna therapy credentialing) charges $3.00 for each mailed check (less for electronic fund transfers). While a $3.00 fee—or a small percentage EFT fee—may seem minor in isolation, these costs accumulate over time. When combined across multiple payers and numerous claims, the total can become a significant financial burden for providers.

(Image of Lady Justice)
Taking Action
What can providers do when they feel fee practices are too great of a burden? Write to the appropriate people: Representatives, Senators, & state Dept. of Insurance (who has insurance regulation oversight). You might even include your governor. You can read a sample letter here. In Texas, there is currently legislation pending passage to reduce these burdensome fees. It was initiated by Rep. Terry Canales, Rep. Tom Oliverson, & Rep. Lacey Hull. (Thank you, Representatives!) Please contact your elected officials to request support for HB 3863 whose goal is to protect providers from avoidable fees & ensure fair payment practices. Specifically, the bill prevents insurers from forcing providers to accept payments through virtual credit cards (VCCs) or any other method that charges extra fees. This ensures providers receive full payment without unnecessary costs.
Note: Though progress has been made with the LTA, more change is needed. Currently, Medicare doesn’t pay separately for training & education related to compression garments — despite the additional time needed to train & educate patients on several issues. Issues like how to don & doff garments, education on available aids that make getting compression on & off easier & how to use them, care of garments, replacement schedule, fit issues (measuring or remeasuring when changes are needed). These issues can take several additional sessions. When you’re not paid for your time & work, it increases burnout.