As a certified lymphedema therapist, one of the most important things to understand (& to help your patient understand) is the difference between edema and lymphedema. While both involve swelling, they have different causes, underlying mechanisms, and treatment needs. Most importantly, proper diagnosis is essential, because if we don’t treat the whole picture, therapy won’t work as well as it should or it may actually even make swelling worse.

What Is Edema?
Edema refers to swelling caused by excess fluid in the body’s tissues. It often results from underlying medical conditions like:
- Congestive heart failure
- Kidney or liver disease
- Venous insufficiency (poor vein function)
- Medications
- Immobility or prolonged sitting/standing
- Hormones
Edema is usually soft, pits easily when pressed, and may improve with elevation or diuretics. It’s caused by issues in the vascular (blood) system and the effect on capillaries. It is not caused by issues with the lymphatic system. Edema sometimes affects the entire body, but often it affects the lower body due to positioning and gravity.
What Is Lymphedema?
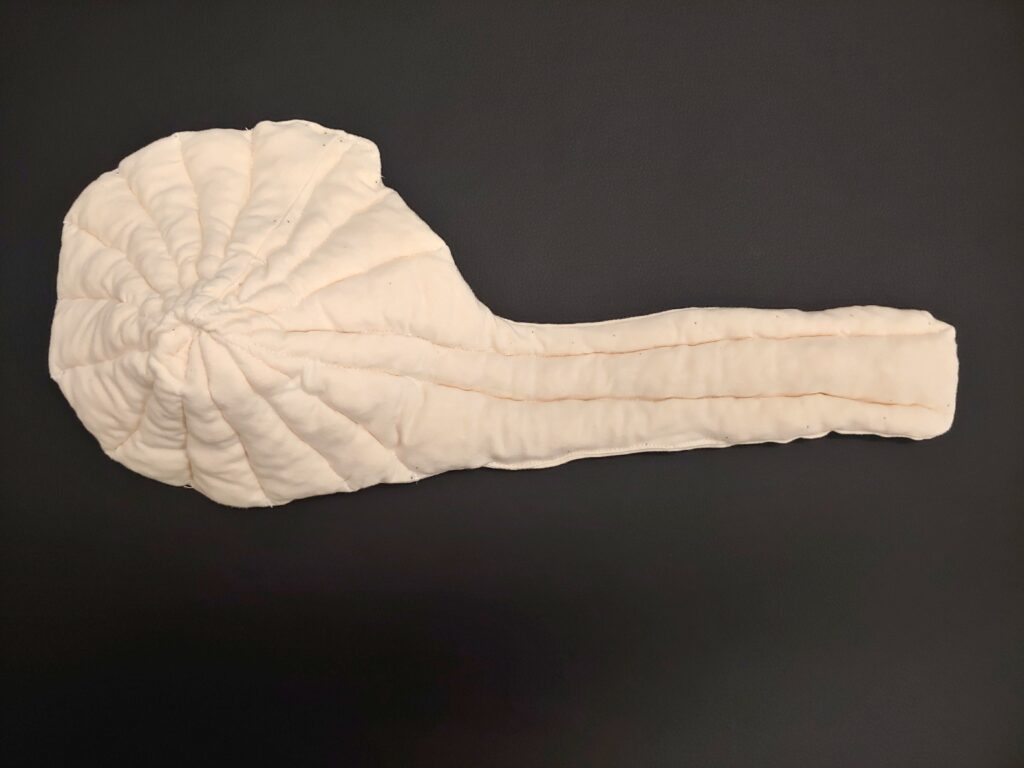
Lymphedema is a chronic condition caused by dysfunction in the lymphatic system. When lymph vessels or nodes are damaged, removed, or malformed, protein-rich fluid builds up in the tissues, leading to persistent swelling — most commonly in the arms or legs.
There are two types:
- Primary lymphedema: A congenital or hereditary issue with lymphatic development.
- Secondary lymphedema: Acquired, often due to surgery, cancer treatment, trauma, or infection.
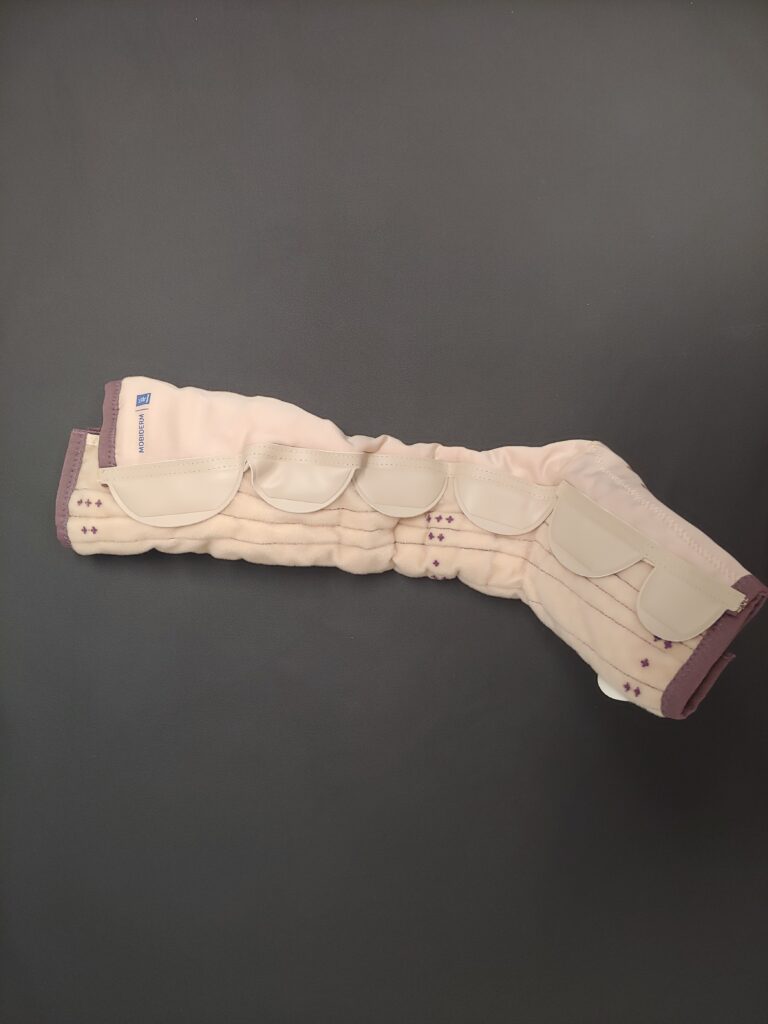
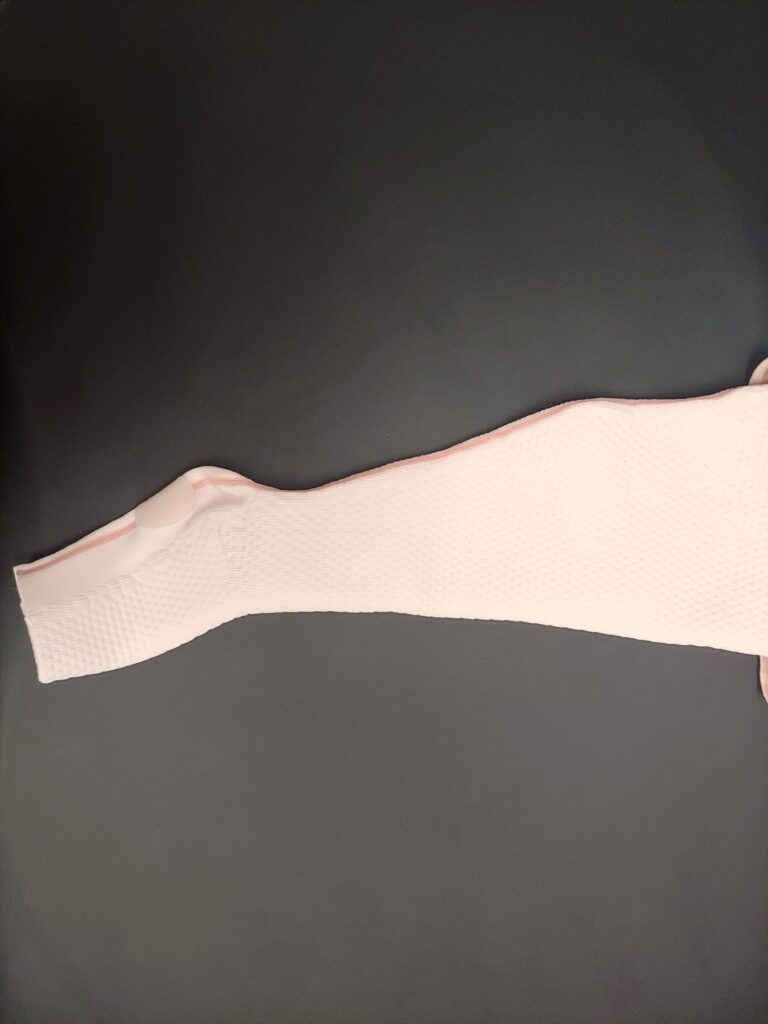
Lymphedema may initially improve with diuretics but diuretics will make lymphedema worse in the long-run. Lymphedema doesn’t resolve on its own. It requires Complete Decongestive Therapy (CDT), a specialized, multi-step treatment approach including manual lymph drainage, compression therapy, skincare, and therapeutic exercise.
When Edema and Lymphedema Coexist
Sometimes, patients have a combination of both edema and lymphedema. For example, chronic venous insufficiency (edema) and secondary lymphedema. This is known as phlebolymphedema. Combined form can be more difficult to manage than lymphedema alone.
Here’s why this matters: when other underlying medical conditions are present and not addressed, CDT by itself won’t be enough (and may even cause harm). As Földi’s Textbook of Lymphology states: If accompanying diseases are undiagnosed and/or untreated, CDT will not be successful.1
This is an essential reminder for both patients and healthcare providers: we can’t treat lymphedema in isolation if other health issues are contributing to the swelling. Whether it’s heart failure, uncontrolled diabetes, or kidney disease, these conditions must be addressed in tandem with lymphedema care.
Why This Matters
Misidentifying edema as lymphedema — or vice versa — can lead to ineffective treatment. Diuretics won’t help pure lymphedema. Compression alone won’t solve swelling due to heart or kidney disease. And CDT may fall short if other conditions are left untreated.
A comprehensive evaluation by a lymphedema therapist and appropriate medical workup can lead to more accurate diagnosis, better treatment plans, and improved outcomes.
Conclusion
If you’re dealing with chronic swelling, don’t settle for a one-size-fits-all explanation. Seek a thorough assessment that looks at the whole picture. When all contributing factors to swelling are treated, we set the stage for long-term success.
References
1 Foldi, M, Foldi, E. (2006). Foldi’s Textbook of Lymphology (2nd ed.), p. 281. Germany: Urban and Fisher.