Last month, we highlighted how therapists can bill insurance for compression for their own patients. It’s not exactly straight-forward. There are several federal & state laws that must be considered (among others). And if you want to bill compression for other people’s patients, well – that throws a wrench into the mix! This post will discuss how therapists can do that & what needs to be considered.
Disclaimer: Information is not guaranteed to be comprehensive or accurate. Consult a healthcare law attorney for guidance.
Billing Medicare
Let’s recap your options for billing for compression as a therapist. There are (3) models.
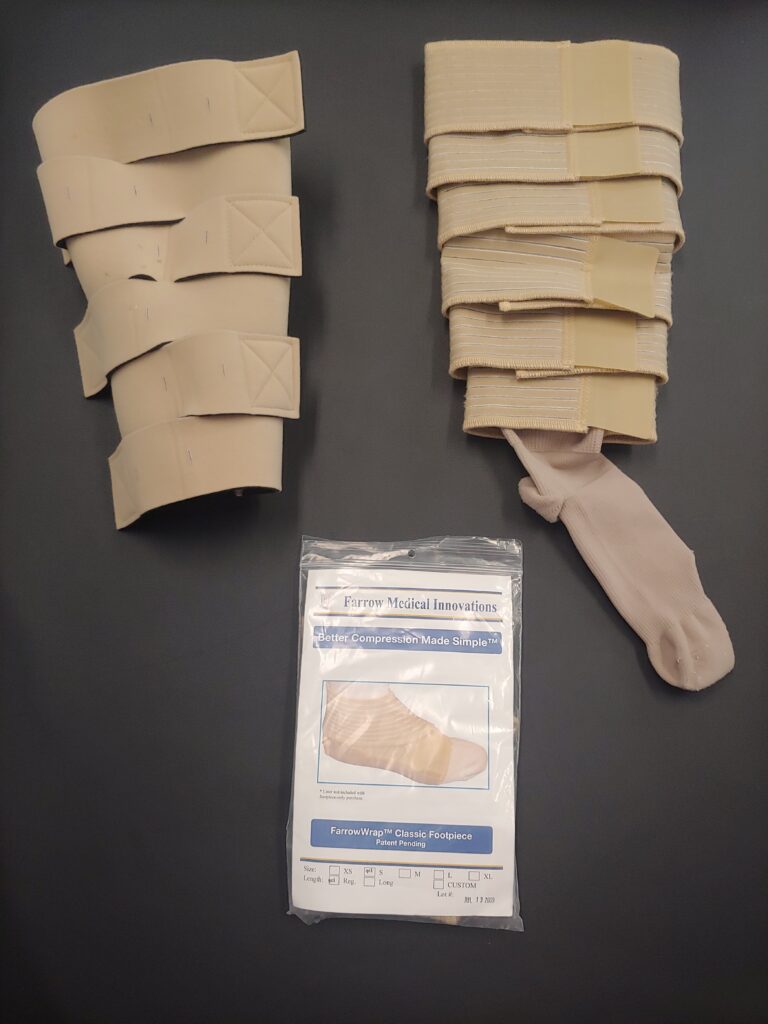
- You only bill Medicare for compression as a supplier (not for service as a provider). You still have to know the laws relevant to DME & pay related fees. But the model is simple.
- You bill Medicare for compression as a supplier & for service as a provider within your business. It’s still fairly simple but it is a bit more complex than the first model.
- You bill Medicare for compression as a supplier & for service as a provider – but you also want to bill compression for other people’s patients. Hmmm….that’s tricky. This model has unique ownership precautions that not only gets into federal statutes (as do the above options) but also criminal liability.
First, in order to bill for compression, you must have a DME license in your state & follow your laws (therapist or not). You must also credential with insurance companies (if you want to be in-network) & decide whether you’re going to bill yourself (using a software) or whether you’re going to use a third-party. (Each of these has their own learning curve.)
Second, if you want to bill for compression in other states (obviously for people who are not your patients), you must follow the same procedures as above. You also need to be prepared to open a physical location in each of those states. Third, if you plan to bill for your own patient’s compression & also bill for other people’s compression, you need to be aware of federal statutes pertaining to fraud & abuse as well as to business ownership.
Federal Statutes: Fraud & Abuse Laws1
The Office of Inspector General outlines five of the most important laws pertaining to medical professionals. These include:
1. False Claims Act – don’t lie, overcharge or provide poor-quality goods
2. The Anti-Kickback Statute – don’t give or take rewards (money or otherwise) for referrals or business involving federal funds
3. Stark (or self-referral) Law – a physician (or their family) can’t have a financial interest in a business & refer Medicare or Medicaid patients to it
4. The Exclusion Authorities – people or business convicted of certain crimes are automatically excluded from federal health care plan participation
5. Civil Monetary Penalties Law – you may be fined fees (ranging from $10k-$50k per violation) based on certain laws breached
Some of these laws are for physicians only (such as Stark Law), but others pertain to everyone. The most relevant to our discussion is the Anti-Kickback Statute. We’ll pick that topic up next time.
References
https://oig.hhs.gov/compliance/physician-education/fraud-abuse-laws/
Attribution
Pexels calculation photo by Tom Miroshnichenko
Pexels gavel photo by Katrin Bolovtsova